Abstract
Introduction: Hyponatremia is a clinical condition which can be summarized when serum sodium is less than 135 mMol/L, it is the most commonly encountered electrolyte imbalance in clinical practice. It is usually associated with poor clinical outcomes including falls, fractures, increased length of hospital stay, institutionalisation and mortality. Prevalence is known to increase in frail patient groups, such as elderly, hospitalised, peri-operative patients with a fracture. Elderly patients with fragility fractures (EPFF) have increased risk of hyponatremia as a result of degenerate physiology, multiple co-morbidities, polypharmacy, increased risk of dehydration due to hospitalisation and peri-operative fluid restriction, and homeostatic stress from fracture and subsequent surgical interventions.
Material and Method: We conducted a prospective interventional study in a tertiary care centre including 43 patients above the age of 60 years (Range 61 years to 90 years) (Mean age 71.23 years) admitted with fragility fracture around hip, which included inter-trochanteric fractures, sub-trochanteric fractures and neck of femur fractures, pubic ramus fracture, mode of trauma strictly being low energy injuries like trivial fall, patients with high energy trauma, and injuries like shaft of femur fracture, acetabular fracture, pelvic ring fractures were excluded from the study.
Results: Amongst 43 patients incidental hyponatraemia was seen in 36(83.72%), with mild (41.86%), moderate (27.90%) and severe (13.95%), incidence of diabetes mellites type 2 was seen in (74.41%), hypertension was (83.72%), chronic kidney disease upto stage 2 was seen in (6.9%) and (18.6%) were hypothyroid, there were (n=13) patients whose comorbidities were noticed after injury. Average duration of hospital stay and Barthel index (scale to measure activity of daily living) showed linear correlation with initial stage of hyponatraemia in patients, with length of hospital stay was average 24.75 days among the severe deficiency group and 15.25 days in normonatremic group, Barthel index was (90 to 100) among the normonatremic patients and less than 70 in patients with initial hyponatremia at 2 weeks from surgery.
Conclusion: With our study we can conclude that we have to look out for electrolyte disturbance, sodium being most common, incidence of fragility fractures with sodium disturbance, can be due to manifestation of osteoporosis, early diagnosis and management can help in preventing as well as in good outcome in such injuries.
Introduction
Hyponatremia is a clinical condition which can be summarized when serum sodium is less than 135 mMol/L, it is the most commonly encountered electrolyte imbalance in clinical practice [1,2]. It is usually associated with poor clinical outcomes including falls, fractures, increased length of hospital stay, institutionalisation and mortality [3]. Prevalence is known to increase in frail patient groups, such as elderly, hospitalised, peri-operative patients with a fracture. Elderly patients with fragility fractures (EPFF) have increased risk of hyponatremia as a result of degenerate physiology, multiple co-morbidities, polypharmacy, increased risk of dehydration due to hospitalisation and peri-operative fluid restriction, and homeostatic stress from fracture and subsequent surgical interventions [5]. They are also at higher risk of complications, making this group of special clinical importance. Hyponatremia itself may be responsible for the fracture. Reports of the prevalence of hyponatremia at admission in EPFF vary widely between 2.8%-26.5%, while 2.6-5.5% develop hyponatremia in the post-operative period. Hyponatremia occurs due to disruption of sodium and water homeostasis, normally maintained by complex multi-system physiological mechanisms. Consequently, there are numerous potential underlying causes of hyponatremia, spanning a broad spectrum of diseases, pharmacotherapy and pathophysiological variants each with different treatment requirements. When very acute or severe, hyponatremia may present with neurological symptoms which can result in serious complications e.g. hyponatraemic encephalopathy, non-cardiogenic pulmonary oedema, seizures, coma, death. However, 75-80% of cases of hyponatremia are mild and chronic (i.e. serum sodium 130-134 mMol/L, occurring over 24 hours) and typically devoid of obvious neurological symptoms [6]. As a result, chronic mild hyponatremia is frequently considered asymptomatic despite being strongly associated with major geriatric conditions and multi-organ pathological changes. These include abnormal gait patterns, falls, fractures, cognitive impairment, bone demineralisation, longer hospital stay, institutionalisation and increased mortality [7]. Despite this, older people may be at lower risk of hyponatraemic encephalopathy and subsequent complications of acute severe hyponatremia, where female gender, hypoxia and liver dysfunction are associated with poorer prognosis [8] whether hyponatremia is an independent predictor of patient outcomes or a marker of disease severity is controversial [9]. Nevertheless, it is very treatable, so its association with multiple poor clinical outcomes is important.
Materials and Methods
We carried out a prospective observational study of all adults aged 65 years or over admitted with a fragility fracture to a university teaching hospital from 7th January – 4th April 2021. Fragility fractures were defined as those occurring either without trauma or due to low energy trauma, equivalent to a fall from standing height or less than one metre. Anonymous baseline data (age, sex, fracture site and admission serum sodium) of all identified EPFF were recorded (Tables 1 and 2).
Table 1: Patient range
|
Age range |
Number of patients |
| 65-70 |
9 |
| 71-75 |
8 |
| 76-80 |
10 |
| 81-85 |
8 |
| 86-90 |
5 |
| Above 90 |
3 |
| Total |
43 |
Table 2: Patients and Serum Na levels
|
Serum Na level at the time of admission |
Number of patients | Serum Na after administration of correction | Serum Na at the time of discharge from hospital |
Mean hospital stay from date of admission in days |
| 135-145 |
7 |
Nil given | >135-140 |
15.25 |
| 131-135 |
18 |
>136-140 | >135-140 |
18.25 |
| 126-130 |
12 |
>130 | >135 |
23.55 |
| 121-125 |
6 |
>130 | >135 |
24.75 |
Inclusion Criteria
We included patients with age more than or equal to 65 years, patients who gave history of trivial trauma, like fall due to slipping of foot, who didn’t gave any history of direct trauma, patients with trauma around hip, so fractures included were inter-trochanteric, sub-trochanteric, pubic ramus fractures also we included neck of femur fractures, patients with medical comorbidities were included and their baseline investigations were done.
Exclusion Criteria
Adults with incapacity were excluded from recruitment and those associated with head injury or any other systemic trauma and with mode of trauma which included high velocity were also excluded. Patients with trauma which required prolonged bed rest were also excluded. Those with any history of metastatic illness were excluded. Participants were recruited from acute orthopaedic trauma wards and a geriatric assessment unit. Clinical data were collected daily until discharge, from patient interview, medical and nursing notes, observation and fluid balance charts and laboratory computer systems by a single investigator. Medication data were obtained by reconciling patient and/or carer histories, and primary and secondary care records. Also, clinical examination of volemic status was performed daily by the investigator. This involved measurement of skin turgor, capillary refill time, mouth moistness, axillary moistness, jugular venous distension, peripheral oedema and overall impression (signs selected based on previous research recommendations) [22]. Examination was carried out by one investigator to increase reliability of findings, maximise consistency and exclude effects of inter-observer variability. Cases of hyponatremia were defined as any serum sodium measurement, 135 mmol/L. An expert panel, consisting of two consultant geriatricians with special interest in hyponatremia and one consultant orthopaedic surgeon reviewed and determined aetiology of each case of hyponatremia. The panel did not examine patients themselves but instead retrospectively reviewed each case of hyponatremia relying on the detailed daily prospectively collected data and clinical examination findings provided by the investigator. This included all clinical information required to determine underlying cause(s) of hyponatremia – history, medications, detailed daily examination, fluid intake and output charts and laboratory results. Collectively, the expert panel used a diagnostic algorithm to determine underlying cause(s) of hyponatremia. The prevalence of hyponatremia upon admission and the incidence of cases developing in hospital were calculated. For incident cases, we recorded whether the hyponatremia was pre- or post-operative. The proportion of participants with known hyponatremia prior to their fracture was calculated by obtaining the last available serum sodium for each patient prior to their admission to hospital. The laboratory is the only public health service laboratory covering the study population so it was unlikely that patients had more recent investigations elsewhere. Prevalence of hyponatremia at discharge was calculated according to the last available serum sodium measurement prior to discharge (Figures 1 and 2).
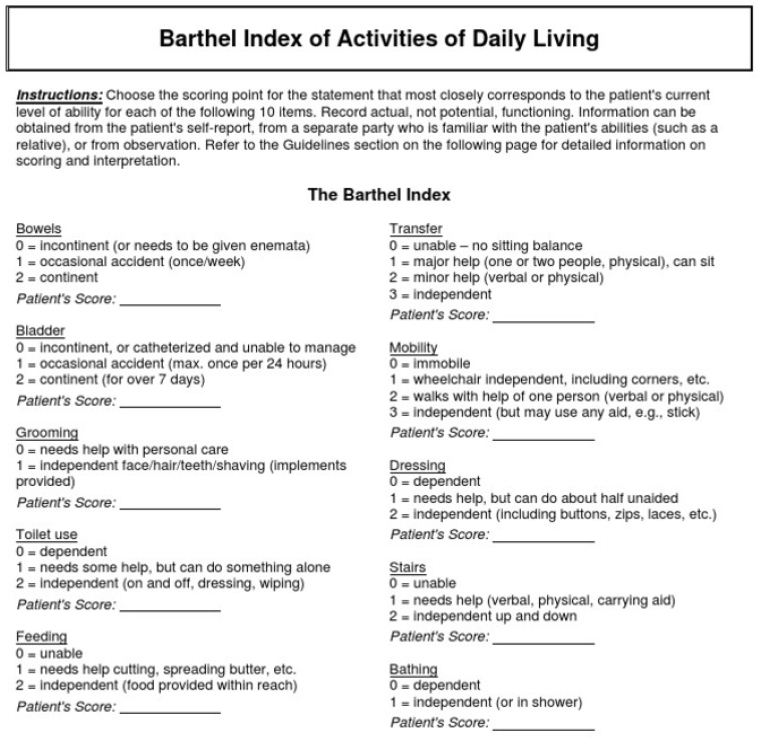
Figure 1: Barthel index of activities of daily living
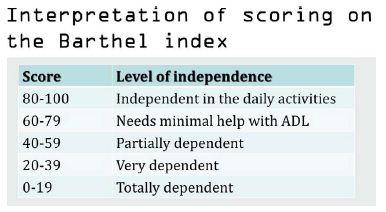
Figure 2: Interpretation of scoring on the Barthel index
Observation and Results
After Recruitment, participant information and data collection there were 167 patients with fragility fractures who presented to our hospital during that period, many of the patients had upper limb fracture mostly dominated by distal radius fracture, after applying our inclusion and exclusion criteria we included total 43 patients in our study. Those not recruited had incapacity to consent, declined participation, or agreed but were later excluded when the original diagnosis of fragility fracture was excluded. There were no statistically significant differences between participants and those who were eligible but declined participation. Amongst the patients we had 43 patients in all, with inter-trochanteric fractures in 10 patients, subtrochanteric fracture in 12 patients and neck of femur fracture in 18 patients and pubic ramus fractures in 3 patients, and among the associated co-morbidities diabetes mellitus type 2 was seen in (74.41%) patients and hypertension in (83.72%) chronic kidney disease upto stage 2 (6.91%) and hypothyroid was seen in (18.6%). Among all the Patients with associated comorbidities who were discovered at the time of admission, and so were not on any medication were total n=13(30.23%). Barthel index for daily activities was noted at the time of dmission, during hospital stay and time of discharge. We noticed we had 7 out of 43 patients who were normo-natremia, 18 patients had mild and 12 mad moderate and 6 had severe hyponatraemia, patients with severe hyponatraemia also had confusion and weakness during peri-traumatic period, and many scholarly articles also have published similar complaints, which was due to hyponatraemia. We noticed that patients with severe hyponatraemia at the time of presentation had mean hospital stay of 24.75 days and those with normo-natremia had mean hospital stay of 15.25 days, there was also similar observation in recovery of the patients with normo-natremia patients having a gradual and sustained increase in Barthel index, due to early mobilisation and shorter duration in trauma to surgery interval with mean od 4.3 days for surgery from trauma and 6.5 days for patients with deranged serum Na levels, for which correction was administered as per general medicine and nephrologist opinion, after serum Na correction there improvement in general condition as well as tolerance to physiotherapy post-surgery. Barthel index was (90 to 100) among the normonatremic patients and less than 70 in patients with initial hyponatremia at 2 weeks from surgery (Figures 3 and 4).
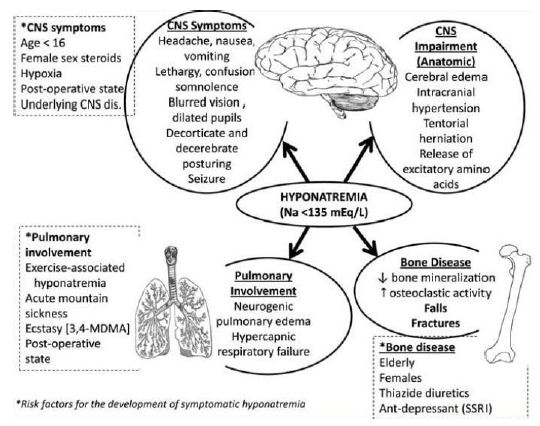
Figure 3: Symptoms
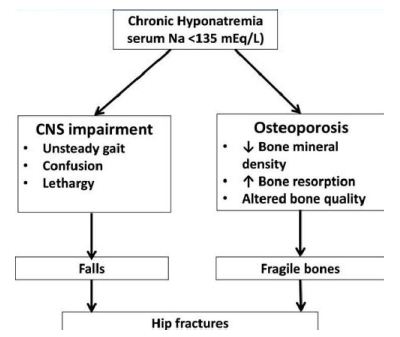
Figure 4: Chronic Hyponatremia
Discussion
We found that, compared to men with serum sodium ≥135 mmol/L men with serum sodium values <135 mmol/L had approximately a 3 fold increase in the risk of hip and incident morphometric spine fractures and a 2½ fold increase in the risk of prevalent morphometric spine fractures. Further, the strength of the relationship between hyponatremia and fractures was not substantially reduced after adjusting for multiple well established fracture risk factors, and in particular, for falls and bone mineral density [10].
Our results are consistent with previous studies that have reported on associations between hyponatremia and fractures. A case control study identified 513 cases of fractures (mainly hip and femoral neck) after a fall and reported an increased risk of fracture, by about 3 fold in men and women with hyponatremia (<135 mmol/L)[11], even after adjusting for medications and medical conditions known to confound that association between fracture and serum sodium. A second case control study reported on the prevalence of hyponatremia (<135 mmol/L) among 364 subjects presenting to the emergency department with fractures of the hip/pelvis and femur compared with the incidence of hyponatremia in 364 controls (subjects presenting to the emergency department with non-critical complaints)[12]. The incidence of hyponatremia in those with fractures was more than double that of controls. A recent cross sectional study by Arampatzis et al. reported that of 10,823 emergency department admissions among adults (≥50 years) there was an increased risk of osteoporotic fracture (OR= 1.46; 95%CI: 1.05 to 2.04) among individuals with diuretic-induced hyponatremia. A secondary data analysis of 1408 women participating in a study of chronic kidney disease determined that those with hyponatremia (again less than 135 mmol/L) had a 2 fold increase risk of fracture (based on self-report) even after adjusting for BMD [13,14].
Our analyses showed similar but generally stronger associations between hyponatremia and fracture risk compared to the only other prospective study of the issue; a secondary analysis performed within the Rotterdam Study that included 5208 men and women of which 399 (9%) had a hyponatremia (serum sodium <135 mmol/L)[15]. In the Rotterdam Study those with hyponatremia there was a 1.4 fold increase in nonvertebral fractures over 7.4 years of follow up and a 1.8 fold increase in prevalent but not incident vertebral fractures or hip fractures. As in our study, adjustment for factors such as disability index and falls did not substantially change the results. Of note, BMD was not associated with low serum sodium in the Rotterdam cohort [16,17].
There are several mechanisms by which low serum sodium might contribute to an increase risk of fracture. Hyponatremia, even when mild as in our study, might increase the risk of falls and fall related fractures by causing gait instability and attention deficits. One study reported that the threshold for gait deficits associated with hyponatremia was 134 mmol/L and 132 mmol/L for attention deficits. In our study we noted that 31% of men with hyponatremia reported falls in the past 12 months compared with 21% of men with serum sodium >135 mmol/L. However, adjusting for baseline fall history did not substantially change the relationship between hyponatremia and fracture.
There is growing evidence to suggest that unrecognized complications of hyponatremia include bone loss and osteoporosis, though the mechanisms by which this occurs is not clear. Cellular and animal data suggest that hyponatremia may have a direct effect on bone. Hyponatremia can directly stimulate osteoclast genesis and osteoclastic resorption without activation of signalling through osteoblasts [18,19]. Finally, it is possible that hyponatremia is a surrogate marker for other causes of fracture. In our study as well as in others, subjects with hyponatremia were older, in poorer health, more likely to report use of relevant medications (such as diuretics, SSRI’s) and have concomitant illnesses such as thyroid disease that increase the risk of fractures. However, in our analyses the associations between hyponatremia and fracture risk was not substantially altered by adjusting for many potential confounding factors including falls suggesting that hyponatremia might be associated with bone quality. Thus, assessment of BMD with DXA in mild hyponatraemic subjects may not represent the best available method to address microstructural skeletal alterations [20].
Our study had some limitations. Most importantly, this was not a randomized trial and as such it is not possible to definitively conclude that low serum sodium causes fractures, and that correcting serum sodium will reduce the risk of fractures. Another limitation of our study was the fact that serum sodium was measured only at baseline.
Our findings suggest that hyponatremia, one of the most common electrolyte abnormalities, is associated with up to a doubling in the risk of hip and morphometric spine fractures. The association we observed was strong despite the low prevalence of hyponatremia in our cohort and was not altered by adjusting for fall history or bone mineral density. Further studies are needed to determine if hyponatremia results in an increase in fractures, the mechanism by which this occurs, and whether treatment of hyponatremia reduces the incidence of fractures.
Conclusion
With our study we can conclude that we have to look out for electrolyte disturbance, sodium being most common, incidence of fragility fractures with sodium disturbance, can be due to manifestation of osteoporosis, early diagnosis and management can help in preventing as well as in good outcome in such injuries. From our study we can also draw a relationship between, hyponatraemia and osteoporosis and also weakness and associated confusion in severe hyponatraemia, though our study is limited with a exclusion of upper limb fragility fracture and also vertebral osteoporotic fractures, we can successfully draw a conclusion regarding early electrolyte restoration post trauma and also a scrutiny in suspected patients for early detection and prevention of such fractures.
References
- Gankam KF, Andres C, Sattar L, Melot C, Decaux G (2008). Mild hyponatremia and risk of fracture in the ambulatory elderly. 101: 583-588 [crossref]
- Tolouian R, Alhamad T, Farazmand M, Mulla ZD (2012). The correlation of hip fracture and hyponatremia in the elderly. J Nephrol 25: 789-793. [crossref]
- Sandhu HS, Gilles E, DeVita MV, Panagopoulos G, Michelis MF (2009). Hyponatremia associated with large-bone fracture in elderly patients. Int Urol Nephrol 41: 733-737.
- Arampatzis S, Gaetcke LM, Funk GC, et al. (2013). Diuretic-induced hyponatremia and osteoporotic fractures in patients admitted to the emergency department. Maturitas 75: 81-86. [crossref]
- Kinsella S, Moran S, Sullivan MO, Molloy MG, Eustace JA (2013). Hyponatremia independent of osteoporosis is associated with fracture occurrence. Clin J Am Soc Nephrol 5: 275-280. [crossref]
- Hoorn EJ, Rivadeneira F, van Meurs JB, et al. (2011). Mild hyponatremia as a risk factor for fractures: the Rotterdam Study. J Bone Miner Res 26: 1822-1828. [crossref]
- Blank JB, Cawthon PM, Carrion-Petersen ML, et al. (2005) Overview of recruitment for the osteoporotic fractures in men study (MrOS). Contemporary clinical trials.26: 557-568. [crossref]
- Orwoll E, Blank JB, Barrett-Connor E, et al. (2005) Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study–a large observational study of the determinants of fracture in older men. Contemp Clin Trials 26: 569-58. [crossref]
- Cauley JA, Blackwell T, Zmuda JM, et al. (2012) Correlates of trabecular and cortical volumetric bone mineral density at the femoral neck and lumbar spine: the osteoporotic fractures in men study (MrOS). J Bone Miner Res 25: 1958-1971. [crossref]
- Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8: 1137-1148. [crossref]
- Mackey DC, Lui LY, Cawthon PM, et al. (2007) High-trauma fractures and low bone mineral density in older women and men. JAMA 298: 2381-2388. [crossref]
- Pahor M, Chrischilles EA, Guralnik JM, Brown SL, Wallace RB, et al. (1994) Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol 10: 405-411. [crossref]
- Bailey IL, Lovie JE (1976) New design principles for visual acuity letter charts. Am J Optom Physiol Opt 53: 740-745. [crossref]
- Levey AS, Stevens LA, Schmid CH, et al. (2009). A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604-612. [crossref]
- Renneboog B, Musch W, Vandemergel X, Manto MU, Decaux G (2006) Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med 119: 7. [crossref]
- Barsony J, Sugimura Y, Verbalis JG (2011) Osteoclast response to low extracellular sodium and the mechanism of hyponatremia-induced bone loss. J Biol Chem 286: 10864-75. [crossref]
- Verbalis JG, Barsony J, Sugimura Y, et al. (2010) Hyponatremia-induced osteoporosis. J Bone Miner Res 25: 554-563. [crossref]
- Hoorn EJ, Liamis G, Zietse R, Zillikens MC (2011) Hyponatremia and bone: an emerging relationship. Nat Rev Endocrinol 8: 33-39. [crossref]
- Lindner G, Pfortmuller CA, Leichtle AB, Fiedler GM, Exadaktylos AK (2014) Age-related variety in electrolyte levels and prevalence of dysnatremias and dyskalemias in patients presenting to the emergency department. Gerontology 60: 420-423. [crossref]
- Adrogue HJ, Madias NE (2000) Hyponatremia. N Engl J Med 342: 1581-1589.