Abstract
Introduction: Cleft palate is a common congenital defect with several described surgical repairs. It is generally an isolated congenital abnormality but can be associated with multiple syndromes. Although there are a multitude of surgical options, many are variations of a previously described repair, and the most successful treatment modality remains a controversy.
Case Summary: The patient, a man, age 25 years old, had a Class III cleft lip and palate Veau classification, underwent a modified palatoplasty and acquired a favourable palatopharyngeal closure function, decreased hemorrhage and swelling.
Conclusion: In this study, we provide a modified palatoplasty for all palate cleft variations, it may benefit for uvula intact, reduce bleeding and swelling.
Keywords
Congenital cleft palate, Modified palatoplasty, Cleft palate repair
Introduction
Cleft of the palate, CP, is one of the most prevalent orofacial birth defects around the world occurring in about 0.33 in every 1000 live births regardless of race, and there was no significant difference between men and women [1,2]. The cleft palate is generally an isolated congenital abnormality but can be associated with other anomalies or multiple syndromes, with or without the presence of lip or alveolar clefting [3]. According to the Veau classification, the cleft palate is divided into four groups depending on the extent of involvement: Group I is limited to the soft palate only; Group II involves the soft and hard palates; Group III includes the soft and hard palate as well as the lip; and Group IV is bilateral complete clefts Figure 1 [4].
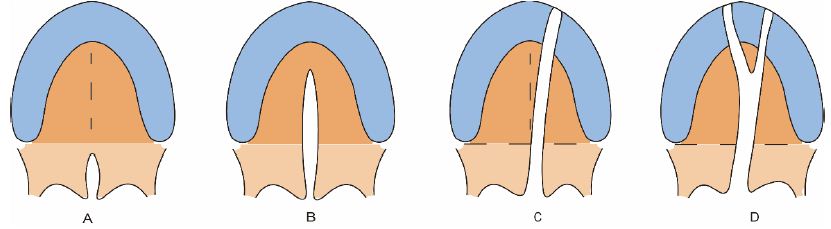
Figure 1: Veau classification. A class I. defects of the soft palate only; B class II. Defects involving the hard palate and soft palate; C class III. Defects involving the soft palate to the alveolus, usually involving the lip; D class IV. Complete bilateral clefts.
Congenital palate defect is caused by disturbed embryonic development when the palatal shelves fail to fuse during the 6th~12th week of pregnancy [5]. It is multifactorial, influenced by genetic factors recessive or incompletely dominant polygenic inheritance and exogenous factors drugs, folic acid deficiency, viral infections, etc [6]. It has been difficult to point to a single etiologic mechanism responsible for this complex trait, resulting in severe speech, nutrition, and mental and social developmental disorders that significantly reduce patients’ quality of life [7].The diagnosis of cleft palate is not difficult because of its obvious features. Treatment of cleft palate ordinarily requires multiple interventions spanning time from birth to adulthood [8]. However, current treatment for this disease generally demands early surgery and face reconstruction procedures that may be revised during childhood and infancy, causing a great number of patient complaints and economic burdens on health systems that need to be minimized [9]. In this study, we report a modified operation of palatoplasty that provides a choice for these patients to shorten operation time, and reduce intraoperative bleeding, trauma, and postoperative swelling.
Case Report
A 25-year-old Chinese man came with a congenital cleft of lip and palate, he received lip repair in the local hospital when he was 4 years old. However, palatal repair was suspended because of a lack of money. Nowadays, the patient was referred to our hospital for palatal cleft repair which significantly affects pronunciation. The patient denied other abnormal parts of the body and his parents are both normal. After comprehensive examination and imaging evaluation by a professional maxillofacial surgeon, he was diagnosed with CP group III, Class III skeletal pattern malocclusion, microdontia, defect of dentition, and dental cavity Figure 2. At this time, the patient only wanted to receive palatal cleft repair.
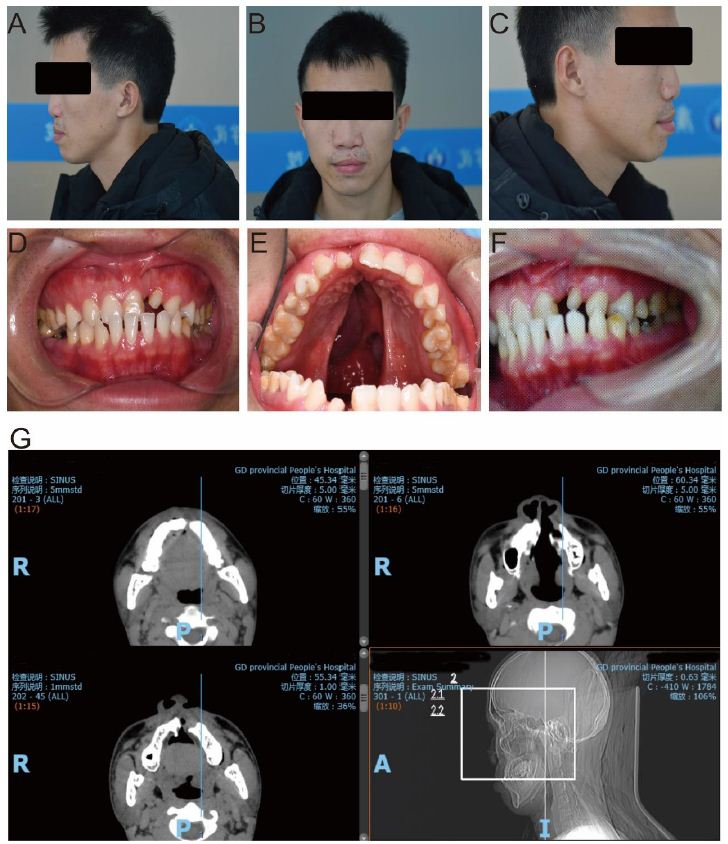
Figure 2: Clinical information of the patient. A-C the profile photo of the patient; D-F the itro-oral film of the patient; G the computerized tomography imaging of the patient.
A cleft of the soft and hard palate with cleft lip postoperative was seen in our patient. Our modified palatoplasty involves: 1. relaxing incisions along the lateral edge of the hard palate, starting anteriorly near the palatomaxillary suture line, going posteriorly just medial to the alveolar ridge, and ending lateral to the hamulus, approximately to the tuberosity of the alveoli. 2. The incision posterior to the maxillary tuberosities was widened by blunt dissection, the hamulus was identified and the hamulus pterygoideus was broken. 3. The mucosa along the edges of the cleft starting at the palatal alveolar to anteriorly 5 mm of uvula was also incised Figure 3A and 3B. 4. The entire mucoperiosteum was then raised from the oral surface of the hard palate; care was taken to preserve the two neurovascular pedicles, the greater palatine pedicle posteriorly and the incisive pedicle anteriorly. Thus, bi-pedicled mucoperiosteal flaps were created on both sides of the cleft Figure 3C. 5. Three layers, including an oral mucosal layer, muscle layer, and nasal layer were dissected which tends to relieve tension on the repair and reduce the postoperative fistula rate. 6. Firstly, the nasal side of the cleft was closed, using redundant mucoperiosteum from the incision along the cleft edge Figure 3D. 7. Secondly, residual mucosa along the edges of the cleft uvula fissa was incised, and seamed the nasal layer. 8. Next, the muscle layer was closed approximately using an intravelar veloplasty. 9. Lastly, the bi-pedicled oral mucosal flaps were approximated to cover the oral surface of the cleft Figure 3E. A month later, the patient returned to our clinic, the palatine mucosa was integrity and the uvula recovered Figure 3F. The speech quality of this man was also improved and had a good velopharyngeal function (Figure 4).
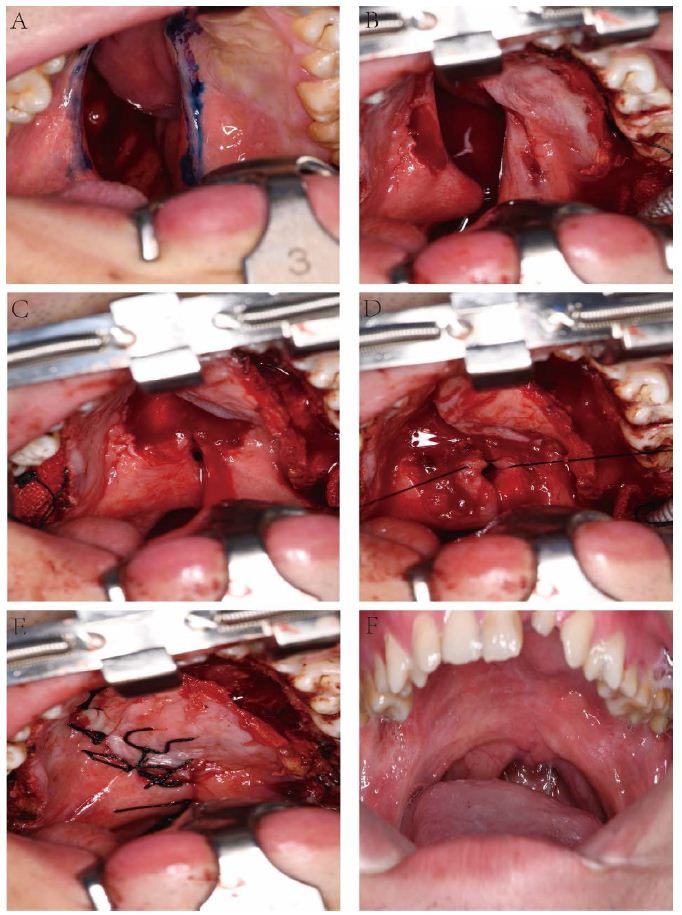
Figure 3: Surgical procedures of the patient and postoperative manifestation. A-E the operative procedues of the patient; F one month postoperative follow-up of the patient.
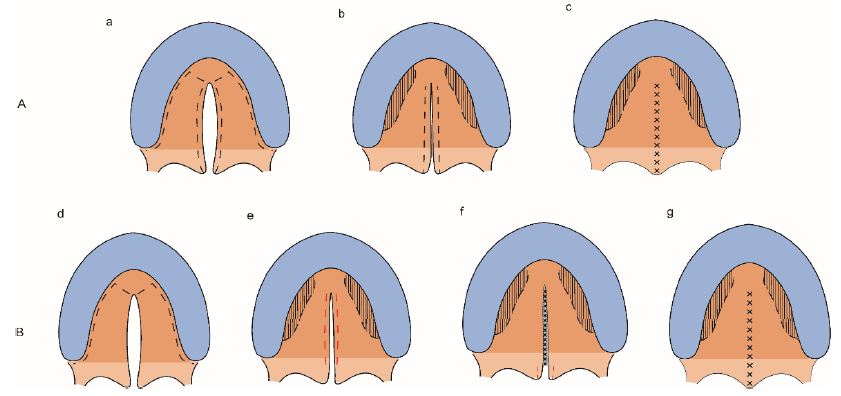
Figure 4: Traditional surgery and modified operation. (A) a-c the traditional surgery of the palatoplasty; (B) d-g the modified surgery of the palatoplasty.
Discussion
The goals of palatoplasty are to acquire complete and intact closure of the palate and restoration of the velopharyngeal sphincter. Besides, reducing hemorrhage, avoiding palatal fistula, and decreasing postoperative swelling also should include care. After decades, there are many techniques for cleft palate repair and each has its advantages. To repair the soft palate, Intravelar Veloplasty, and Furlow Double-Opposing Z-Plasty are widely applied [10,11]. To repair the hard palate, the Von Langenbeck Palate palatoplasty, Veau-Wardill-Kilner palatoplasty, Two-Flap palatoplasty, and Vomer Flap techniques are employed around the world [11-14]. Nonetheless, the most successful treatment modality remains controversial. According to Veau classifications, surgeons are recommended to choose appropriate surgical techniques for the patients after evaluating the results as they see fit to provide the best functional outcomes for their patients [15]. However, all the techniques above mentioned may cause uvula injury due to incision without suture immediately and improve the occurrence of velopharyngeal incompetence. The rate of oronasal fistula following primary cleft palate surgery was about 3.8~6.1% [16]. In this study, we raise a modified palatoplasty: delayed incision of the uvula and earlier suture of the nasal layer. It is beneficial for uvula integrity, reducing uvula tears, and decreasing hemorrhage and swelling.
Fusion of particular orofacial structures during early gestation is required for proper development of the upper lip and jaw. Failure of this process leads to an orofacial cleft, which manifests as a gap in the tissue of the upper lip, the palate, or both [17]. Treatment of cleft lip and palate ordinarily requires multiple interventions spanning the time of birth to adulthood [18]. This process includes a multidisciplinary evaluation, involving pediatric dentists, oral and maxillofacial surgeons, orthodontists, prosthodontists, speech therapists, and psychological consultation teachers. In this study, our patient only underwent the necessary surgery because of financial difficulty, we sincerely advise he achieve serial therapy shortly.
Conclusion
We preferred the modified palatoplasty for all cleft variations. The use of modified palatoplasty in the cleft palate seems to contribute to a reduction of hemorrhage, uvula varies, and postoperative swelling.
Acknowledgement
Cailing Jiang contributed to the conception, design, analysis and interpretation of data, and drafting of this article. Chong Jiang, Zijun Guo and Haiyou Wang contributed to data collection and analysis. Sui Jiang contributed to the conception and design, critical review of the article, and final approval.
Declaration
The authors declare no conflict of interest.
Funding
The preparation of this manuscript was not supported by any funding or grants.
Ethics Approval
Ethics approval was received from the ethics committee of Guangdong Provincial People’s Hospital (KY2023-827-03).
References
- Salari N, et al. (2022) Global prevalence of cleft palate, cleft lip and cleft palate and lip: A comprehensive systematic review and meta-analysis. J Stomatol Oral Maxillofac Surg 123: 110-120. [crossref]
- Aframian DJ, RV Lalla, DE Peterson (2007) Management of dental patients taking common hemostasis-altering medications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103: S45 e1-11. [crossref]
- van Aalst JA, KK Kolappa, M Sadove. (2008) MOC-PSSM CME article: Nonsyndromic cleft palate. Plast Reconstr Surg 2008. 121: 1-14. [crossref]
- Oliver JD, et al. (2021) Innovative Molecular and Cellular Therapeutics in Cleft Palate Tissue Engineering. Tissue Eng Part B Rev 27: 215-237. [crossref]
- Lewis CW, et al. (2017) The Primary Care Pediatrician and the Care of Children With Cleft Lip and/or Cleft Palate. Pediatrics 139: 5. [crossref]
- Candotto V, et al. (2019) Current concepts on cleft lip and palate etiology. J Biol Regul Homeost Agents 33: 145-151 [crossref]
- Lindeborg MM, et al. (2020) Optimizing speech outcomes for cleft palate. Curr Opin Otolaryngol Head Neck Surg,28: 206-211. [crossref]
- Ruscello DM,LD Vallino. (2020) The Use of Nonspeech Oral Motor Exercises in the Treatment of Children With Cleft Palate: A Re-Examination of Available Evidence. Am J Speech Lang Pathol 29: 1811-1820 [crossref].
- Frederick R, et al. (2022) An Ideal Multidisciplinary Cleft Lip and Cleft Palate Care Team. Oral Dis 28: 1412-1417. [crossref]
- Furlow LT, Jr.1(1986) Cleft palate repair by double opposing Z-plasty. Plast Reconstr Surg 78: 724-38. [crossref]
- LaRossa D. (2000) The state of the art in cleft palate surgery. Cleft Palate Craniofac J 37: 225-8. [crossref]
- Pigott RW, et al. (2002) A comparison of three methods of repairing the hard palate. Cleft Palate Craniofac J 39: 383-91. [crossref]
- Elander A, et al. (2017) Isolated cleft palate requires different surgical protocols depending on cleft type. J Plast Surg Hand Surg 51: 228-234. [crossref]
- Mommaerts MY, KK Gundlach, A Tache. (2019) “Flip-over flap” in two-stage cleft palate repair. J Craniomaxillofac Surg 47: 143-148. [crossref]
- Liu H, et al. (2021) A new congenital cleft palate New Zealand rabbit model for surgical research. Sci Rep 11: 3865.
- Bykowski MR, et al. (2015) The Rate of Oronasal Fistula Following Primary Cleft Palate Surgery: A Meta-Analysis. Cleft Palate Craniofac J 52: e81-7. [crossref]
- Rossell-Perry P. (2022) Regarding a Personal Strategy for Cleft Palate Repair. J Craniofac Surg 33: 725-726. [crossref]
- Lane H, S Harding,Y Wren. (2022) A systematic review of early speech interventions for children with cleft palate. Int J Lang Commun Disord 57: 226-245. [crossref]