According to the Institute of Medicine [1], the desired goal of patient-centered health care is for practitioners to be “respectful of and responsive to individual patient preferences, needs, and values” (Institute of Medicine, 2001, para. 1) [1]. Patient-centeredness relies on effective communication [2]. Dialogue is essential for health care settings, requiring the patient to receive important information from the medical professional, as well as the medical professional understanding and responding to important information that the patient conveys. Research has shown that better health care outcomes are achieved when patients have a positive relationship and interaction with their health care provider [3]. However, when patients identify with a culture and use a first language that is different from their health care provider, they may experience service and information barriers when seeking medical treatment, resulting in less adherence to treatment plans or avoidance of seeking medical care [4]. The exchange of medical information, even at routine office visits, can become perilous when the patient cannot fully participate in discussions regarding safe uses of medications, or complex, even risky, decision-making expectations (Hedding & Kaufman, 2012), A medical appointment with a deaf patient without appropriate communication accommodations can result in miscommunication, misinformation, misdiagnosis, and mistrust. Deaf people often experience inequities in health care which lead to poor health (Barnett et al., year) and lower health literacy (significant gaps in basic health knowledge) than their non-deaf counterparts [5]. Too often, medical appointments for deaf patients continue without the use of an interpreter, due in part to a lack of awareness by providers of the importance of communication accommodation or the lack of available interpreters (Ebert & Heckerling, 1995, as cited in [6]. This combination of potential lower health literacy, lack of interpreters, and health care providers who are unaware or unprepared to meet this population’s specific needs highlights the frustration of countless deaf people. The exchange of medical information, even at routine office visits, can become perilous when the patient cannot fully participate in discussions regarding safe uses of medications, or complex, even risky, decision-making expectations (Hedding & Kaufman, as cited in Swabey & Malcom, 2012) [6].
Faculty of two distinct programs at a large midwestern university created an opportunity to experience patient-centered service provision with deaf volunteers. Nursing faculty wanted their students to experience the dynamics of engaging patients who are deaf and use American Sign Language (ASL) as their primary language. Deaf people whose primary language is ASL, which is distinct from English with its own complex grammar and distinct syntax, vocabulary, and discourse style [7], require special communication access considerations. Simulation in health care education is designed to replicate real clinical situations in a safe environment. The International Nursing Association for Clinical Simulation and Learning (INACSL) states that the specific purpose of simulation is to “promote, improve, or validate a participant’s performance” [8]. Validating the importance of simulation, some nursing boards have approved up to 100% replacement of traditional clinical hours with simulation in specialty areas such as pediatric and obstetrical nursing [9,10]. Thus, simulation can be a bridge between classroom and clinical environments and as a venue in which to address communication access concerns for deaf patients.
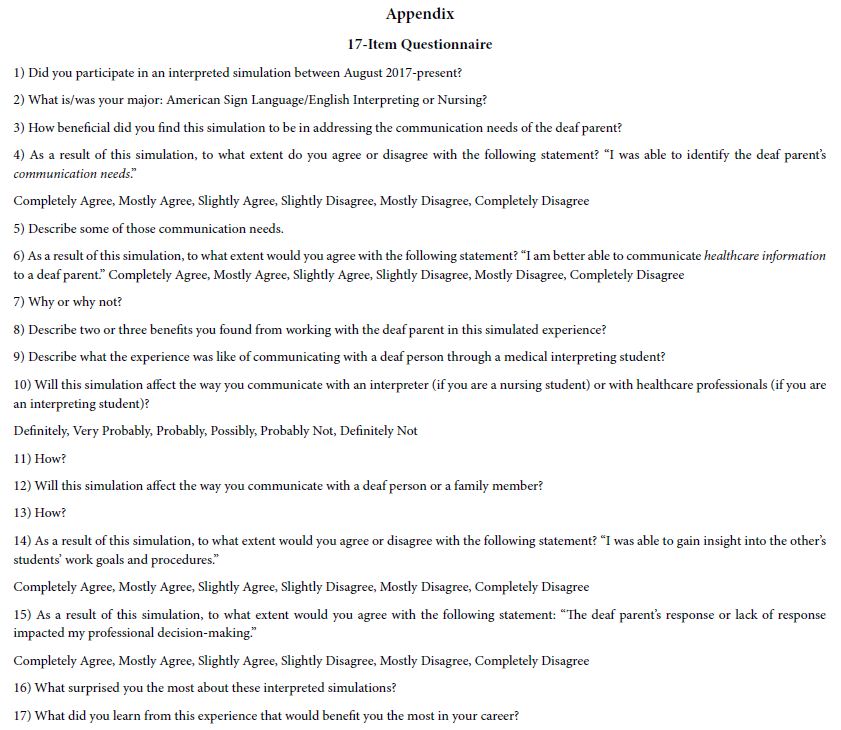
The scenario lasted 20 minutes. During the first 10 minutes, nursing students performed a comprehensive physical exam. After approximately 10 minutes, students were encouraged to begin discharge teaching with interpreting students to facilitate communication with the deaf parent. After that, the 20-minute debriefing session began. Interpreting students reversed roles at this point. The debriefing was facilitated by an experienced nurse who gave each group of students a series of questions to discuss. In order to compare the perceived effectiveness of the simulation, a Mann-Whitney test statistic was calculated. Two questions were posed to participants that evaluated their self-perception of the effectiveness of the simulation. The first, “I am better able to communicate healthcare information to a deaf parent” was rated on a Likert-scale (1: completely disagree; 2: mostly disagree; 3: slightly disagree; 4: slightly agree; 5: mostly agree; 6: completely agree). Results indicated a statistically significant difference between groups of students (U=173.00, p=0.020), indicating that nursing students (Median=6) were more likely to agree with the question than interpreting students (Median=5). The second question, “Will this simulation affect the way you communicate with a deaf person or their family member?” was also rated on a Likert-scale (1: definitely not; 2: probably not; 3: possibly; 4: probably; 5: very probably; 6: definitely). However, the difference between Nursing (Median=5) and interpreting students (Median=5) was not statistically significant (U=83.50, p=0.195).
Results were statistically significant for both the first (D=0.270, p<0.001) and second (D=0.258, p<0.001) prompt, indicating that a randomly selected response from this sample is significantly more likely to be positive than negative on either prompt. Nursing students were more likely to provide the highest rating regarding ability to communicate healthcare information to deaf parents than interpreting students. This simulation experience allowed nursing and interpreting students to understand and appreciate the role of the other and to enact strategies to improve communication. Both groups of participants found the simulated experience to be beneficial and felt it gave them a safe environment in which to practice. Faculty initiating this partnership recognized many potential benefits to both programs in preparing their students to provide services to deaf people in a specialized setting. Nursing students were able to work with individuals who processed language in a different way than they were accustomed to. Interpreting students were able to relate medical information to deaf people in a realistic, dynamic, and unrehearsed setting. Both interpreting and nursing students’ responses were positive, stating the advantages of practicing vital nursing and communication skills with a deaf parent in a safe environment. Collaboration among interpreting and nursing students in simulation may enhance understanding and provide authentic practice opportunities of unique accommodations to achieve patient-centered health care.
References
- Institute of Medicine (2001) Committee on quality of health care in America. Crossing the quality chasm: A new health system for the 21st century. National Academies Press.
- Barnett S, McKee M, Smith SR, Pearson TA (2011) Deaf sign language users, health inequities, and public health: Opportunity for social justice. Preventing Chronic Disease 8. [crossref]
- Raymond CW (2014) Conveying information in the interpreter-mediated medical visit: The case of epistemic brokering. Patient Education and Counseling 97: 38-46. [crossref]
- Messias DK, McDowell L, Estrada RD (2009) Language interpreting as social justice work: Perspectives of formal and informal healthcare interpreters. Advances in Nursing Science 32: 128-143. [crossref]
- Pollard RQ, Barnett S (2009) Health-related vocabulary knowledge among deaf adults. Rehabilitation Psychology 54: 182-185. [crossref]
- Swabey LA, Malcolm M (2012) In our hands: Educating healthcare interpreters. (Gallaudet University Press).
- Valli C, Lucas C, Mulrooney K, Villanueva M (2011) Linguistics of American Sign Language: An introduction (5th ed.). (Gallaudet University Press).
- INACSL Standards Committee. (2016, December). INACSL Standards of Best Practice: SimulationSM Participant evaluation. Clinical Simulation in Nursing 12(S) (December, 2016): S26-9.
- Ohio Administrative Code, Chapter 4723-5 (2017). Nursing Education Programs. Ohio Board of Nursing.
- Iezzoni L, O’Day BL, Killeen M, Harker H (2004) Communicating about health care: Observations from persons who are deaf or hard of hearing. Annals of Internal Medicine 140: 356-362. [crossref]