Abstract
Arachnoid cysts are spaces containing cerebrospinal fluid partitioned into an arachnoid-formed sheath and are a rare cause of symptomatic spinal cord compression. This case study examined a patient with spastic paraparesis who underwent surgery to remove the cystic lesion and push back the marrow. Post-op control spinal MRI showed total excision of the cyst, and the patient has progressed well and has fully recovered from his deficit.
Nabors divides extradural arachnoid cysts into three types: type 1, type 2, and type 3. Type 1 is essentially thoracic, extending over several vertebrae with a peak of greater frequency around the eighth dorsal vertebra. Symptoms are generally slowly progressive, but rapid revelation or decompensation are possible. Treatment options include marsupialization, wide resection, and total excision. For symptomatic cases, total excision is the reference treatment. For painful cases, complete excision, tied off the intradural communication pedicle, and reshaping the dura is the primary surgical goal.
Keywords
Arachnoid cyst, Spastic paraparesis, Decompensation
Introduction
Arachnoid cysts are commonly defined as spaces containing cerebrospinal fluid partitioned into an arachnoid-formed sheath. Described for the first time by Magendie in 1843 [1]. However, they represent a rare cause of symptomatic spinal cord compression [2]. Their development would require the presence of a communication pathway with the subarachnoid spaces by means of a small opening. This opening could remain open, form an anti-reflux valve, or close completely and then give rise to true cysts. Communicating cysts are also called “arachnoid diverticula” [3]. We report the case of a symptomatic spinal arachnoid cyst that was operated on in our department.
Definition
Arachnoid cysts are arachnoid formations with arachnoid walls that don’t look different from the arachnoid tissue around them. They can develop wherever there is arachnoid tissue, with a tendency to localize in the cisterns, but spinal localization remains rare. These cysts contain CSF of the same composition as the neighboring CSF and communicate with the contiguous arachnoid lakes, allowing regular exchange of intracystic fluid.
Materials and Methods
We have collected a case of symptomatic extradural intraspinal arachnoid cysts that required complete excision with ligation of the intradural communication pedicle and dural plasty.
Case Study
A young 36-year-old patient who has had spastic paraparesis for a few months, whose radiological exploration with a sagittal (a) and axial (b) T2 MRI showed a cystic lesion at the height of D10 D11 with the same signal as the lateralized extradural CSF on the left and driving back the spinal cord on the right.
The patient underwent surgery where a laminectomy was performed, removing this voluminous arachnoid cyst (black arrow) and pushing back the marrow on the right (white arrow). d: reduction of the cystic volume by puncture and coagulation of the cystic wall, which is made of a thick arachnoid. After complete excision of this cyst, we find good release of the marrow (white arrow) and the nerve roots (black arrows). A post-op control spinal MRI shows total excision of the arachnoid cyst; the patient has progressed well and has fully recovered from his deficit (Figure 1).
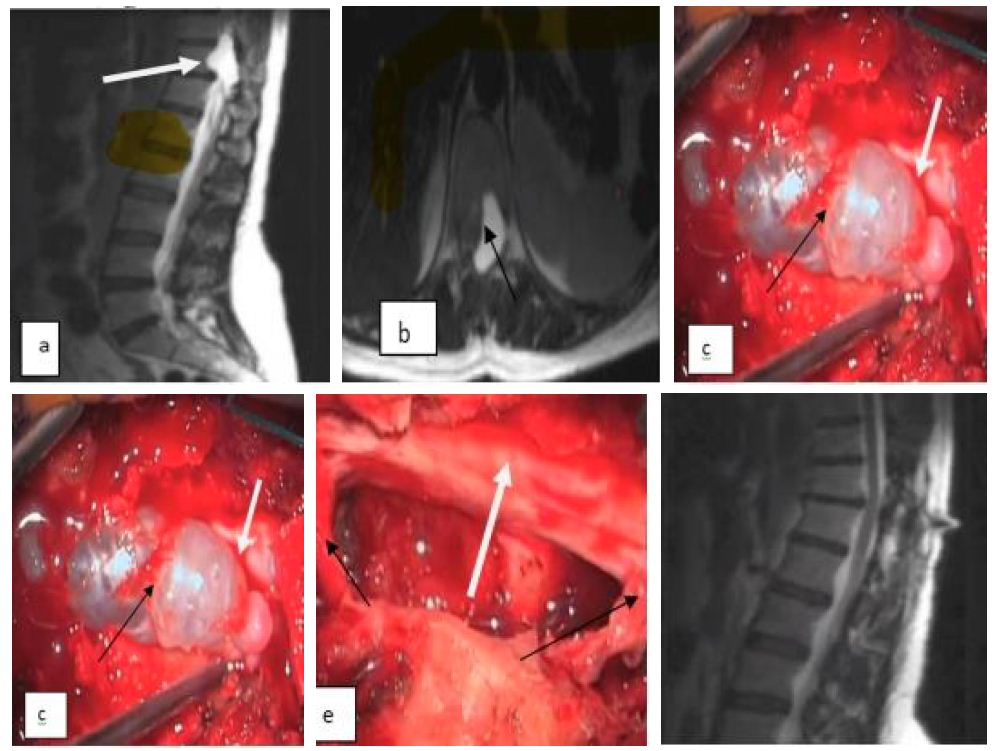
Figure 1: Radiological images sagittal (a) and axial (b) T2 MRI showed a cystic lesion (c), (d) reduction of the cystic volume by puncture and coagulation of the cystic wall. After cyst removal (e) good release of the marrow (white arrow) and the nerve roots (black arrows), (f) post-op control spinal MRI.
Discussion
The term “arachnoid cyst” is used to describe most types of cysts that involve the arachnoid. Nabors [4] has put them into groups based on where they are in relation to the nervous system in:
Type 1: An extradural cyst not comprising a nervous structure;
Type 2: Extradural cyst comprising nervous structures (Tarlov cyst);
Type 3: Intradural cyst.
Its topography is essentially thoracic, extending over several vertebrae with a peak of greater frequency around the eighth dorsal vertebra; our case sits at the level of D10 D11. Cervical or lumbosacral localization is very rare [5]. Dorsal locations are particularly frequent in the second decade of life given the narrowness of the canal at this level, and lumbosacral locations are observed later, between 30 and 50 years of age [6,7]. It is almost exclusively posterior, more rarely anterior or anterolateral [8,9].
In our case, the seat is posterolateral:
There is no sex ratio; the age of discovery can vary from 4 to 80 years, according to the cases listed in the literature [8]. Our patient was 36 years old; the symptoms are generally slowly progressive, but rapid revelation or decompensation is possible [10]; There is no relationship between the severity of the signs and their date of appearance. For thoracic cysts, the duration of the development of symptoms is shorter than for lumbar cysts due to the difference in the diameter of the spinal canal [11];
There are some particularities in terms of their clinical expression: The spinal syndrome and the radicular syndrome are very often in the foreground, frequently increased by the standing position (which may correspond to a tensioning of the cyst or its stretching) [12,13]; spinal deformities are the prerogative of old cysts; the sublesional syndrome, linked to the position of the cyst, is dominated by posterior cord involvement; sphincter disorders are more rare and moderate.
The etiopathogenesis remains hypothetical, and several theories have been presented. Extradural arachnoid cysts likely have a congenital origin, and they are the result of congenital dural diverticula or herniation of the arachnoid through congenital dural aplasia [14]. The nerve or the junction of the dural root and sheath are the most common sites of these defects, although less often the dorsal midline of the dural sac is also involved. The defect of the dura mater would be due to a structural anomaly of congenital origin, the consequence of a failure of the tightness of the collagen fibers. This failure leads to elongation and ectasia of the dura mater. Cases of spinal arachnoid cysts that do not clearly have a congenital origin have also been reported. The association of spinal arachnoid cysts with arachnoiditis potential source of arachnoid septations), spinal surgery, and spinal cord trauma has prompted some authors to suggest that these cysts may result from acquired dural lesions [15]. Several surgical methods can be proposed, including marsupialization of the cyst which consists in opening the cyst and making its contents widely communicated with the spaces under perimedullary arachnoids, however, wide resection of the cyst is the method of choice. Since the goal is to stop the pressure difference between the cyst and the space under arachnoid.
For asymptomatic patients, it is recommended to observe conservative treatment with monitoring of the evolution of clinical symptoms and radiological controls regular. Regarding symptomatic epidural arachnoid cysts, all authors agree on the indication for surgery. It is then recommended to carry out the complete excision of the cyst, and then the pedicle connecting the cyst to the subarachnoid space and the cyst is tied off. repair of the dural defect. This is the technique of choice to prevent the CSF reaccumulation and cyst recurrence. For our patient with a painful extradural arachnoid cyst, we removed the whole cyst, tied off the intradural communication pedicle, and reshaped the dura.
Conclusion
Extradural spinal arachnoid cysts are rare lesions, and treatment options should be considered carefully. In symptomatic cases, total excision of the cyst should be considered the reference treatment. We believe that closure of the dural defect should be the primary surgical goal to prevent recurrence. We offer laminoplasty for the treatment of extradural arachnoid cysts involving multiple segments to prevent postoperative kyphosis.
References
- Perret G, Green D, Keller J (1962) Diagnosis and treatment of intradural arachnoid cysts of the thoracic spine. Radiology 79: 425-429. [crossref]
- Lesoin F, L Eys D, Rousseaux M, Cama A, Jomin M, Petit H (1985) Spinal intradural arachnoid cysts. Acta Neurchir 76 : 125-128.
- Goyal RN, Russell NA, Benoit BG, Belanger JM (1987) Intraspinal cysts: a classification and literature review. Spine 12(3): 209-213. [crossref]
- Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, et al. (1988) Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 68(3): 366-377. [crossref]
- AJNS – African Journal of Neurological Sciences | » KYSTE ARACHNOÏDIEN EXTRADURAL RACHIDIEN AJNS 2009. 28(1).
- Paramore CG (2000) Dorsal arachnoid web with spinal cord compression: variant of an arachnoid cyst? Report of two cases. Journal of Neurosurgery: Spine 93(2): 287-290. [crossref]
- Rimmelin A, Clouet PL, Salatino S, Kehrli P, Maitrot D, et al. (1997) Imaging of thoracic and lumbar spinal extradural arachnoid cysts: report of two cases. Neuroradiology 39(3): 203-206. [crossref]
- LVISI C, ERISOLI M, IULIONI M, UERRA L (1987) Long term results of surgically treated congenital intradural spinal arachnoid cysts. J Neurosurg 67 : 333-335. [crossref]
- Kendall BE, Valentine AR, Keis B (1982) Spinal arachnoid cysts: clinical and radiological correlation with prognosis. Neuroradiology 22(5): 225-234. [crossref]
- Rousseaux M, Combelles G, Destée A (1983) Diverticules et kystes arachnoïdiens rachidiens intraduraux: 6 observations. Neurochirurgie 29: 279-284.
- Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, et al. (1988) Updated assessment and current classification of spinal meningeal cysts. J Neurosurg 68(3): 366-377. [crossref]
- YS, RS, MS (1991) Spinal intradural arachnoid cysts. Neurochirurgia (Stuttg) 1 Juill. 34(4): 127-130. [crossref]
- Ar W, Jd L, Fc K (1975) Septum posticum cysts: an uncommon cause of chronic back pain. Pain 1(3): 271-275. [crossref]
- Neo M, Koyama T, Sakamoto T, Fujibayashi S, Nakamura T (2004) Detection of a dural defect by cinematic magnetic resonance imaging and its selective closure as a treatment for a spinal extradural arachnoid cyst. Spine 29(19): E426-430. [crossref]
- Saqui AE, Aggouri M, Benzagmout M, Chakour K, Chaoui ME (2017) Une cause rare de compression médullaire: kyste arachnoïdien épidural rachidien (à propos de 03 cas). The Pan African Medical Journal. [crossref]