Objective
This article is to differentiate the MRI findings between Parkinson’s disease and Multiple sclerosis. Therefore, this article focuses mainly the brain imaging only.
Case Report
An elderly gentleman- Mr C, diagnosed with vascular dementia was subjected to MRI due to decline in neuromotor function. He had recent symptoms of headache and reduced cognition. A diagnosis of Parkinsons or Parkinson Plus syndrome was made.
The MRI Brain sequence are as follow:
Axial: proton-density and/or T2 FLAIR/T2-weighted.
Sagittal: T2 FLAIR.
Gad contrast enhanced T1-weighted imaging.
Salient features in the T2/FLAIR MRI were reported as deep white matter hyperintensity that were asymmetrical, located primarily at periventricular and juxtacortical regions. Precontrast images show the lesions are hypointense on T1WIs with the “Dawson’s fingers” appearance. And post contrast images show enhancing white matter lesions (Figure 1).
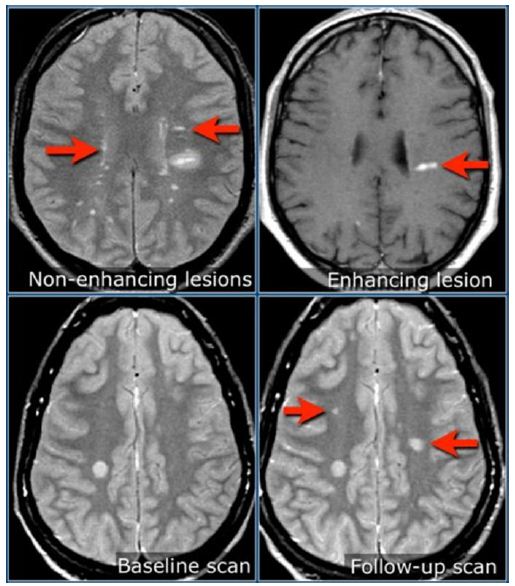
Figure 1: An example of similar lesions- as no patient consent taken for release of original images
Other key points were:
Some lesions being greater than 5 mm.
Some lesions were perpendicular.
Incomplete rim enhancement in larger lesions- gadolinium contrasted.
Further MR cervical spine was suggested to examine for additional lesions. A repeat MRI in 6-12 months was recommended, as new lesions on repeat imaging are common and not all lesions enhance simultaneously at onset. Also suggested for Visual Evoked Potential (VEP) to identify subclinical demyelination.
Discussion
Parkinson Disease (PD), is a neurodegenerative disease and movement disorder characterised by a resting tremor, rigidity and hypokinesia due to progressive degeneration of dopaminergic neurons in the substantia nigra [1-4]. It is characterised by nigrostriatal dopaminergic degeneration leading to neuronal loss in the substantia nigra, most conspicuous in the ventrolateral tier of neurons, and a number of other regions including parts of the basal ganglia, brainstem, autonomic nervous system and cerebral cortex. Upon MRI, loss of the normal swallow tail appearance of susceptibility- signal pattern in the substantia nigra- on axial imaging in a 3T is perhaps the most promising diagnostic sign. Apart from these changes, the signal intensity in substantia nigra depends on loss of neuromelanin and iron accumulation. In addition to aiding diagnosis, MRI is also used to identify features which may indicate secondary parkinsonism rather than primary disease, such as extensive small vessel ischaemic change.
Parkinson-plus syndrome refers to a loose group of neurodegenerative disorders that are characterised by features of Parkinson disease but with other neurological symptoms/signs. They have a poor response to levodopa, and mostly have fairly characteristic neuroimaging features.
Conditions included in Parkinson-plus syndrome include:
- progressive supranuclear palsy (PSP)
- multisystem atrophy (MSA)
- dementia with Lewy bodies (DLB)
On the contrary, Multiple sclerosis (MS) is an inflammatory demyelinating condition.
In MS, the loss of myelin, is accompanied by a disruption in the ability of the nerves to conduct electrical impulses to and from the brain. This produces the various symptoms of MS. The sites where myelin is lost appear as plaque or lesions. In multiple sclerosis, these scars appear at different times and in different areas of the brain and spinal cord. The term multiple sclerosis itself means ‘many scars’. For some, MS is characterised by periods of relapse and remission while, for others, it has a progressive pattern.
Conclusion
The final conclusion of the case based on the MRI appearance was multiple sclerosis. However, a differential diagnosis of Parkinson/Parkinson Plus syndrome was not null and void as the MRI was performed on a 1.5 T machine. However, it is a clinical judgement nevertheless.
References
- Martina Absinta, Sati P, Masuzzo F, Nair G, Sethi V, et al. (2019) Association of Chronic Active Multiple Sclerosis Lesions with Disability In Vivo. JAMA Neurology 76: 1474-1483. [crossref]
- Okuda D, Mowry E, Beheshtian A, Waubant E, Baranzini SE, et al. (2009) Incidental MRI Anomalies Suggestive of Multiple Sclerosis: The Radiologically Isolated Syndrome. Neurology 72: 800-805. [crossref]
- Lövblad K, Anzalone N, Dörfler A, Essig M, Hurwitz B, et al. (2010) MR Imaging in Multiple Sclerosis: Review and Recommendations for Current Practice. AJNR Am J Neuroradiol 31: 983-989. [crossref]
- https://www.ninds.nih.gov/health-information/disorders/multiple-sclerosis