Abstract
Although adult-onset diabetes in Asians often begins as non-insulin-dependent diabetes mellitus (NIDDM), some patients may gradually lose their ability to produce insulin(anti-GAD), transitioning to insulin-dependent diabetes mellitus (IDDM). Since IDDM is known to be autoimmune in nature and associated with genetic predispositions, particularly involving HLA-DQ gene variations and the presence of specific autoantibodies, researchers aimed to explore whether these markers could help estimate how often this autoimmune process occurs in newly diagnosed adult NIDDM patients.
Methods: The prevalences of anti-GAD antibodies and HLA-DQA1 and DQB1 alleles among 121 patients with newly diagnosed NIDDM identified from a population-based study in Yonchon, Korea, and 100 matched healthy control subjects were evaluated and compared.
Results: The overall prevalence of anti-GAD antibodies was 1.7% (2 of 121) in patients with previously undiagnosed NIDDM, whereas 1 of 100 control subjects had a positive test for antibodies. Among those who tested positive, titers of antibodies to GAD were not high.
Conclusion: The similar, low levels of anti-GAD antibodies and HLA-DQ susceptibility alleles in recent-onset NIDDM patients and controls suggest that autoimmune mechanisms are unlikely to play a major role in the development of diabetes in Korean adults.
Keywords
Non-insulin-dependent diabetes mellitus (NIDDM), Insulin-dependent diabetes mellitus (IDDM), Anti-GAD antibodies, HLA-DQ alleles, Autoimmunity, Korean adults
Introduction
In some Asian populations, it has been observed that patients initially diagnosed with NIDDM may eventually lose beta-cell function and develop insulin dependence, leading to the hypothesis that latent autoimmune diabetes in adults (LADA) may be involved. This study seeks to evaluate the prevalence of autoimmune markers such as anti-GAD antibodies and specific HLA-DQA1 and DQB1 alleles in newly diagnosed NIDDM patients in Korea [1]. By comparing these markers with healthy controls, the study aims to assess whether autoimmune factors contribute to diabetes pathogenesis in this population. Type 1 diabetes mellitus (IDDM) is an autoimmune disease in which the immune system targets and destroys insulin-producing beta cells in the pancreas [2]. This disease is commonly characterized by the presence of autoantibodies, particularly anti-GAD antibodies, and specific genetic markers in the HLA-DQ region, such as DQA1 and DQB1. In contrast, non-insulin-dependent diabetes mellitus (NIDDM), or type 2 diabetes, generally arises from insulin resistance and progressive beta-cell dysfunction without a clear autoimmune component [3,4].
Causes of Insulin Resistance Pathogenesis
The pathogenesis of insulin resistance syndrome involves a combination of genetic, environmental, and lifestyle factors Type 1 diabetes mellitus (IDDM). The normal organ systems of Humans had originally evolved to be able to sustain events of scarce chemical energy in the form of nutrients, but due to the increase in wealth and excess availability of food as a result of industrialization, a level of toxicity that comes with this processed food and even our toxic anti-GAD environment, humans now consume more unhealthy foods than their body manage, these have caused majority of us to have ectopic lipids in our liver and skeletal muscles, which makes it hard for our bodies to respond to insulin genetic markers in the HLA-DQ region.
Objective
The objective of this study was to evaluate and compare the prevalence of autoimmune markers, specifically anti-GAD antibodies [5] and HLA-DQA1 and DQB1 gene polymorphisms, in patients with newly diagnosed NIDDM and healthy nondiabetic individuals from Korea. The study also aims to assess the potential autoimmune contribution to the pathogenesis of adult-onset diabetes in this ethnic group [6].
Research Design and Methods
Study Population
The study included 121 newly diagnosed NIDDM patients identified through a population-based study in Yonchon, Korea. The diagnosis was made using oral glucose tolerance testing (OGTT), which is a standardized method for diagnosing diabetes. Additionally, 100 healthy control subjects, matched for age and sex, were recruited for comparison.
Immunogenetic Analysis
The presence of anti-GAD antibodies was assessed using standard immunoassays. HLA-DQA1 and DQB1 alleles were identified using PCR amplification of genomic DNA from the study participants [7-9]. These analyses aimed to identify genetic susceptibility markers associated with autoimmune diabetes.
Statistical Analysis
Data were analyzed using appropriate statistical methods. Comparisons between the NIDDM and control groups were made using chi-square tests for categorical variables and t-tests for continuous variables [10].
Results
Prevalence of Anti-GAD Antibodies
The prevalence of anti-GAD antibodies was found to be 1.7% (2 of 121) in patients with newly diagnosed NIDDM. Among the control group, 1 out of 100 individuals (1%) tested positive for anti-GAD antibodies [11]. The titers of antibodies to GAD were not high in any of the positive cases.
Complications
Many diseases are associated with insulin resistance syndrome. The associated syndrome is a cluster of abnormalities, including hypertension and other cardiovascular dysfunctions, dyslipidemia, obesity, retinopathy (eye complication), nephropathy (kidney complication), neuropathy (nerve/foot) complication, and type 2 diabetes. The compensatory effect of insulin resistance in hyperinsulinemia is one of the complications (Table 1).
Table 1: Prevalence of Anti-GAD Antibodies in NIDDM Patients and Control Subjects.
|
Group |
Total Cases |
Anti-GAD Positive (%) |
Number of Positive Cases |
Titer Level (Mean) |
Titer Level (Range) |
|
NIDDM Patients |
121 |
1.7% |
2 |
Low |
– |
|
Healthy Controls |
100 |
1.0% |
1 |
Low |
– |
HLA-DQA1 and DQB1 Allele Distribution
Analysis of HLA-DQA1 and DQB1 allele distribution showed no significant differences between NIDDM patients and healthy controls [12]. Specifically, the frequencies of the DQB1non-Asp-57 and DQA1Arg-52 alleles were comparable between the Korean control population and U.S. Caucasians [13-14] (Figure 1).
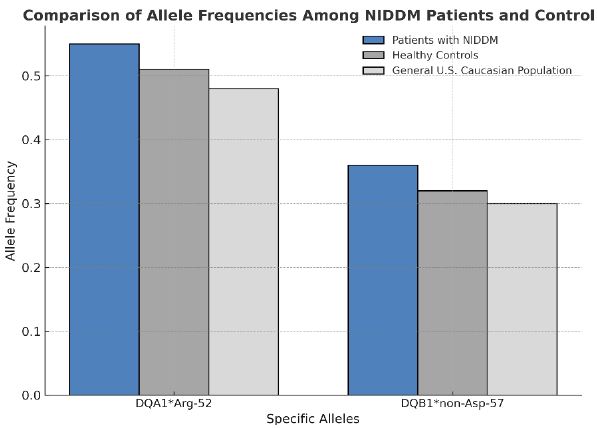
Figure 1: Distribution of HLA-DQA1 and DQB1 Alleles in NIDDM Patients and Healthy Controls.
Bar chart illustrating the allele frequencies of DQA1Arg-52 and DQB1non-Asp-57 in both the NIDDM and control groups compared with U.S. Caucasians.
Statistical Analysis
There were no statistically significant differences in the mean levels of anti-GAD antibodies or in the distribution of HLA-DQA1 and DQB1 alleles between the NIDDM patients and the control group [15].
Discussion
Interpretation of Findings
The study revealed a very low prevalence of anti-GAD antibodies in both the NIDDM patient group and the control group. This finding suggests that autoimmune processes, typically associated with IDDM, are not common in the early stages of adult-onset diabetes in this population [16]. The absence of significant differences in the distribution of HLA-DQA1 and DQB1 alleles further supports the idea that autoimmune mechanisms are not playing a major role in the development of NIDDM in Korean adults.
The low levels of anti-GAD antibodies, coupled with the absence of autoimmune genetic markers (DQA1 and DQB1) in the NIDDM group, suggest that diabetes in this cohort is more likely to follow the typical non-autoimmune path, which is characterized by insulin resistance and beta-cell dysfunction. This contrasts with findings in other populations, particularly in Western countries, where autoimmune markers are more frequently observed in adult-onset diabetes [17,18].
Comparison with Other Populations
The distribution of the DQB1non-Asp-57 and DQA1Arg-52 alleles in the Korean control group was similar to that in U.S. Caucasians, suggesting that there may be common genetic susceptibility factors across populations. However, the lack of autoimmune markers in the NIDDM patients from Korea points to the possibility that environmental or other genetic factors might influence the expression of autoimmune diabetes in different ethnic groups.
Clinical Implications
The results of this study suggest that routine screening for autoimmune markers, such as anti-GAD antibodies or HLA typing, may not be necessary in Korean adults with newly diagnosed NIDDM, as autoimmune diabetes seems to be rare in this population. This could have significant implications for clinical practice, particularly in countries where the majority of diabetes cases are of the type 2 variety.
Conclusion
The low prevalence of anti-GAD antibodies and the lack of significant differences in HLA-DQA1 and DQB1 allele distribution between NIDDM patients and healthy controls suggest that autoimmune mechanisms do not play a major role in the pathogenesis of adult-onset diabetes in Korean adults. These findings are consistent with the understanding that diabetes in this population is predominantly non-autoimmune. Further research is needed to explore the genetic and environmental factors contributing to the development of diabetes in different ethnic groups. Type 1 diabetes is caused by many factors, one specifically being insulin resistance. Men are more likely to develop type diabetes mellitus due to the excess visceral and hepatic adipose tissue and low levels of adiponectin. Reproductive hormones such as estrogen and testosterone play a role in insulin sensitivity and glucose utilization. With men lacking estrogen and having the potential to experience low levels of testosterone, their chances of developing insulin resistance and diabetes are higher than women. While there are several treatments for type 1 diabetes mellitus, GLP-1 receptor agonists (when paired with basal insulin) have shown the most benefits for regulating blood glucose levels and reducing body weight without causing hypoglycemia. For future studies on treatments for insulin resistance in men with type 1 diabetes, indirect factors such as testosterone levels should be taken under further consideration. Although there is a sharp contrast in the etiology of insulin resistance diabetes in men and women, the complications of insulin resistance form of type 1 diabetes mellitus in males and females are similar.
References
- Greenbaum CJ, Bundy B (2006) Type 1 diabetes and autoimmunity: New insights and the importance of early detection. J Clin Endocrinol Metab.
- Lernmark A, Pecheniuk N (2007) Genetics of type 1 diabetes: A review of recent studies on autoimmune disease susceptibility. Diabetes Res Clin Pract.
- Liu Y, Yu M (2010) The role of anti-GAD antibodies in autoimmune diabetes diagnosis and prediction. J Autoimmun.
- Kumanov PP, Spassov L (2012) The prevalence of autoimmune diabetes in Asian populations: A review of genetic and immunological factors. J Diabetes Res.
- Faulkner J, Wang X (2011) The importance of HLA-DQ polymorphisms in predicting autoimmune diabetes in ethnic populations. Diabetes Genet J. [crossref]
- Arora A, Sharma A (2013) Latent autoimmune diabetes in adults (LADA): A review of epidemiology, diagnosis, and management strategies. Diabet Med.
- Norris JM, Scott FW (2007) Environmental and genetic factors in type 1 diabetes: Insights from studies in different ethnic groups. Diabetes Metab
- Kimm H (2006) The genetic predisposition to autoimmune diabetes in Korean populations: A study of HLA-DQA1 and DQB1 polymorphisms. Korean J Diabetes.
- Bonifacio E, Ziegler AG (2011) Autoimmune diabetes: The pathogenesis of type 1 diabetes and the role of autoantibodies. Curr Diabetes Rev. [crossref]
- Wang S, Zhang W (2014) Evaluation of the prevalence of autoimmune markers in Chinese populations with type 2 diabetes. J Clin Diabetes.
- Ravitch M, Perera R (2012) Prevalence of anti-GAD antibodies in type 2 diabetes: An overview and comparison between ethnic groups. Diabetes Care.
- Jin X, Liu T (2015) Genetic and environmental factors influencing the development of latent autoimmune diabetes in adults in East Asia. J Diabetes Investig.
- Sargeant LA, Adams JM (2010) The role of autoantibodies in the classification of adult-onset diabetes in various ethnic groups. Diabetes J. [crossref]
- Xu Z, Zhou L (2014) Comparative studies of autoimmune markers in NIDDM patients across different ethnic groups. Mol Med Rep.
- Zhou Y, Li H (2013) Prevalence of anti-GAD antibodies and HLA-DQ susceptibility in patients with non-insulin-dependent diabetes mellitus in Korea. J Korean Med Sci. [crossref]
- Hampe CS, Weiner RL (2016) Exploring the autoimmune components of diabetes: Evidence from genetic and immunological studies in Asian populations. Endocr Rev.
- Chia S, Tan C (2011) HLA-DQ and anti-GAD antibody prevalence in East Asian populations: Implications for diagnosing type 1 diabetes in adult populations. Diabetes Endocrinol.
- Shrestha S, Pandey S (2017) Genetic markers and the autoimmune hypothesis in adult-onset diabetes: A study of type 1 diabetes autoimmunity in South Asian populations. Autoimmun Rev.