Abstract
Objective: To conduct a systematic review and analysis of the risk factors linked to sepsis in adult trauma patients, providing evidence-based medical evidence for reducing the incidence of sepsis following trauma.
Methods: Literature searches were conducted in the total of 9 databases from their inception to December 2023 on factors influencing sepsis in trauma patients. Meta-analysis was conducted using the meta package in R, and the model’s heterogeneity was assessed using the I² value.
Results: A total of 10 literatures were included, involving 65,866 adult patients admitted for trauma, with 5,165 cases of sepsis following trauma. The meta-analysis results showed that advanced age (MD=1.31,95%CI: 0.51~ 3.12), male gender (OR=1.21, 95%CI: 0.95~1.54), Injury Severity Score (ISS) (MD=5.99, 95%CI: 3.05~8.93), Glasgow Coma Scale (GCS) score (MD=-1.75, 95%CI: -2.68~-0.81), Acute Physiology and Chronic Health Evaluation (APACHE II) score (MD=4.37, 95%CI: 2.56, 6.17), Sequential Organ Failure Assessment (SOFA) score (MD=2.51, 95%CI: 2.30~2.73), mechanical ventilation (OR=4.71, 95%CI: 3.44, 6.45), blood transfusion (OR=2.20, 95%CI: 1.63~2.96), central venous catheterization (OR=2.74, 95%CI: 1.93~3.89), concurrent shock (OR=2.30, 95%CI: 1.70~3.10), and emergency surgery within 24 hours (OR=2.85, 95%CI: 2.00~ 4.07), were identified as independent risk factors for sepsis among trauma patients.
Conclusion: Sepsis in trauma patients is influenced by a variety of risk factors. Clinical medical staff should intervene early in High-risk patients with these factors should be targeted to reduce sepsis incidence among trauma patients.
Keywords
Trauma, Sepsis, Risk factors, Meta-analysis
Introduction
Trauma represents a major global health burden, accounting for around 9% of annual deaths and ranking among the leading causes of mortality worldwide [1]. The advent of advanced medical technologies has successfully curbed the early mortality rate among trauma patients. However, a significant number of survivors are at risk of developing sepsis in the days or weeks following the initial trauma [2]. Sepsis, a complex clinical syndrome arising from a dysregulated host response to infection, not only can precipitate septic shock and multiple organ failure but also substantially worsens the prognosis [3]. The development of sepsis is associated with an overactive and persistent inflammatory response in trauma patients and is a prevalent complication [4]. Existing studies have reported that the mortality rate among trauma patients with sepsis hovers between 17% and 23% [5], highlighting the gravity of this complication. Despite a plethora of research efforts, the majority of which are based on single-center data, there remains a lack of consensus regarding the identification of specific risk factors for sepsis in trauma patients.
Meta-analysis, a powerful tool that aggregates and quantifies the effect sizes of individual studies through systematic review, emerges as a promising approach to address this issue [6]. By comprehensively reviewing and dissecting the extant literature on the risk factors associated with post-traumatic sepsis, this study aims to systematically organize and deliberate upon these factors. The ultimate goal is to furnish a robust evidence-based foundation for clinical practice, thereby facilitating the early detection and prevention of sepsis in trauma patients and potentially ameliorating their outcomes.
Methods
Protocol and Registration
This research adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [7] and our systematic review protocol was recorded on PROSPERO (International Prospective Register of Systematic Reviews, with the registration number CRD42024537479). As the data utilized were publicly accessible, ethical committee approval was not pursued.
Retrieval Strategy
Literature Sources and Search Strategy Literature was retrieved from databases including China National Knowledge Infrastructure, Wanfang Data, China Science and Technology Journal Database, China Biology Medicine Literature Database, PubMed, Embase, Web of Science, Cochrane, CINAHL, and Scopus from their inception to December 2023. We utilized the keywords included trauma, traumatic, post-traumatic, multiple injuries, polytrauma, septic, sepsis, septicemia, multiple organ failure, factor, and risk. Databases for dissertations and trial registries were not searched. The specific search strategies employed for English databases are detailed in Appendix 1.
Inclusion and Exclusion Criteria
Inclusion criteria: 1) Age ≥18 years; 2) Study population consisting of trauma patients; 3) Sepsis diagnosed according to Sepsis-1, Sepsis-2, or Sepsis-3 criteria; 4) Independent risk factors determined through multivariate regression analysis. Exclusion criteria: 1) insufficient patient baseline data; 2) reviews, meta-analyses, commentaries, case reports, guidelines, letters, conference abstracts, and literature related to animal experiments; 3) abnormal data and/or not conforming to statistical rules. The predominant literature reviewed comprised case- control and retrospective cohort studies, predominantly authored in either English or Chinese. We excluded smaller studies (those with fewer than 50 patients) to avoid potential false negative results. Additionally, patients with burns were excluded because they have distinct risk factors, such as a compromised skin barrier, which could potentially elevate the risk of developing sepsis [8].
Literature Screening and Data Extraction
Search results were imported into EndNote X9 software (Clarivate Analytics, London, UK) for management. Two independent reviewers (Wang B and Shi Y) screened titles and abstracts against predefined inclusion/exclusion criteria, following Cochrane guidelines. Potentially relevant citations were subjected to full-text review. Data extraction was performed independently from all eligible studies using a standardized form, with a third researcher consulted to resolve any discrepancies. The main extracted content included: principal investigator, study design, publication region and year, sample size, characteristics of the study population (age, sex), follow-up period, identified risk factors, and outcomes of multifactorial regression analysis.
Quality Assessment of Literature
Two researchers (Zhu X and Dong C) independently assessed the quality of the literature using the Newcastle-Ottawa Scale (NOS) [9]. NOS scores categorized the literature into three quality levels: ≥7 (high quality), 4-6 (moderate quality), and <4 (lower quality). In the event of any disagreements during the assessment process, the opinion of a third researcher (Cao S) will be sought to resolve them.
Statistical Analyses
Statistical analyses were conducted using Review Manager (version 5.3), STATA (version 12.0), and the ‘meta’ package in R software. The categories of subgroup analyses of incidence included: age, year of publication, research region, diagnostic criteria for sepsis, and duration of follow-up. For categorical variables, the Odds Ratio (OR) and 95% Confidence Intervals (CI) were used to express the statistical effect size, while the Mean Difference (MD) and 95% CI were used for continuous variables. Heterogeneity across studies was evaluated with the intraclass correlation index (I²), which quantifies the proportion of total variation in study outcomes due to between-study variance (τ²) rather than chance [10]. I² ≥ 50% was considered indicative of significant heterogeneity. In these instances, a random-effects model was employed for meta-analysis; otherwise, a fixed-effects model was applied. Publication bias was assessed via Egger’s regression test and funnel plots, with P < 0.05 considered statistically significant.
Results
Study Characteristics
A preliminary collection of 3391 articles was obtained, and a total of 10 articles were ultimately included (Figure 1). The 10 articles included in this study were all retrospective cohort studies [11-20], published between 2004 and 2023. Upon summarizing the literature, there were 12 risk factors with ≥2 articles, including 10 articles on age [11-20] as a risk factor; 9 articles on male gender [11-19] as a risk factor; 8 articles on Injury Severity Score (ISS) [12-18,20] as a risk factor; 5 articles each on Glasgow Coma Scale (GCS) [13,14,17,18,20] Sequential Organ Failure Assessment (SOFA) [11,13-16], mechanical ventilation [13-17], and shock [12,14-17]as risk factors; 4 articles each on Acute Physiology and Chronic Health Evaluation II (APACHE II) [11,13,14,16], number of blood transfusions [13,15-17], and emergency surgery within 24 hours [13,15-17] as risk factors; 3 articles each on central venous catheterization [14-16] and diabetes [11,12,20] as risk factors. The study characteristics are shown in Table 1.
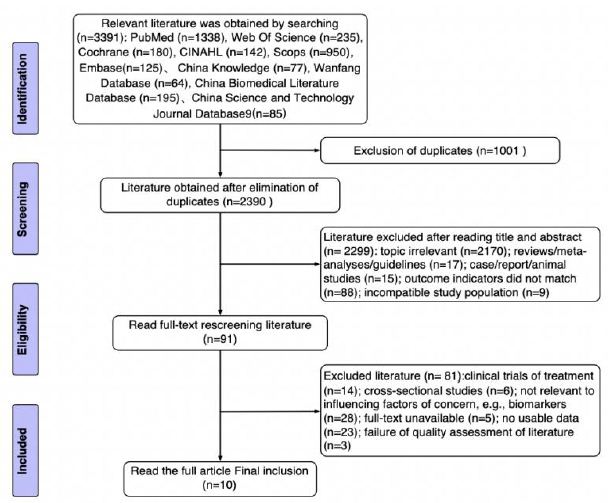
Figure 1: PRISMA diagram for identification of relevant studies. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1: Baseline characteristics of studies included for analysis
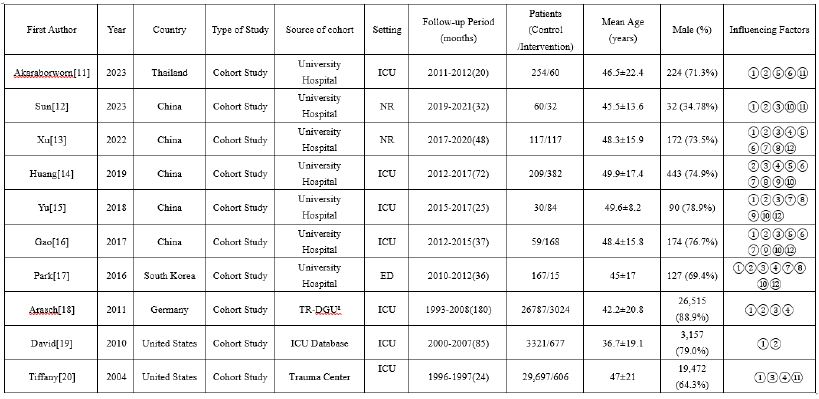
Note:① Age (years); ② Sex (Male); ③ Injury Severity Score, ISS; ④ Glasgow Coma Scale, GCS; ⑤ Acute Physiology and Chronic Health Evaluation II, APACHE II; ⑥ Sequential organ failure assessment, SOFA; ⑦ mechanical ventilation, MV; ⑧ blood transfusion; ⑨ Central venous catheterization, CVC; ⑩ Shock: SBP < 90 mmHg at hospital; ⑪ Diabetes; ⑫ Emergency surgery: surgery within 24 hours.
aTR-DGU: Trauma Registry of the German Society for Trauma Surgery
NR: not reported
Outcomes of Incidence and Subgroup Analyses
There were 65,866 trauma inpatients, with 5,165 cases of sepsis and 60,701 cases without sepsis. The I² was 100%, so a random-effects model was used. The results showed that the incidence of sepsis in adult trauma patients was 35.2% (95% CI: 17.8%, 52.7%) (Figure 2). Subgroup analyses were conducted based on age, publication year, study region, sepsis diagnosis criteria, and follow-up duration. The results showed: subgroup analysis by continent demonstrated a pooled incidence rate for the age group 30≤Age < 69 years was the highest at 37.9% (95% CI: 19.8%, 58.0%); when grouped by publication year, the incidence rate for the group after 2020 was 34% (95% CI: 15%, 56%), lower than the incidence rate for the group before 2020, which was 38.6% (95% CI: 22.9%, 55.6%); subgroup analysis by study region, the incidence rate was 60.1% (95% CI: 48.0%, 71.5%) in China, higher than the incidence rate in other regions was 10.3% (95% CI: 4.2%, 18.5%); when grouped by sepsis diagnosis criteria, the incidence rate for the group using the third edition of sepsis diagnosis criteria was 60.1% (95% CI: 48.0%, 71.5%), higher than the group using the first and second editions of sepsis diagnosis criteria; when grouped by follow-up duration, the incidence rate for the group with a follow-up duration of 32 to 72 months was the highest at 45.2% (95% CI: 22.5%, 68.9%). Supplemental Table 1 for details.
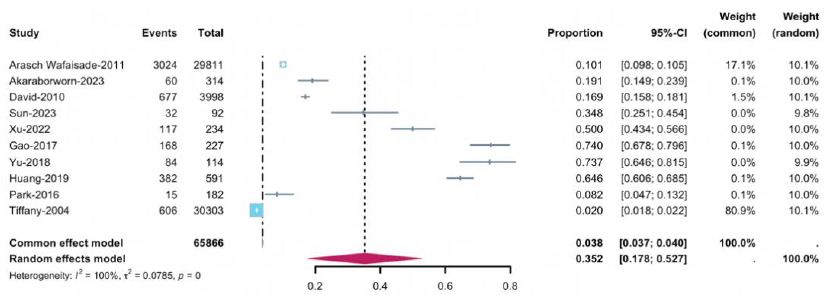
Figure 2: Forest plot of the incidence of sepsis in trauma patients
Outcomes of Sepsis Influencing Factors
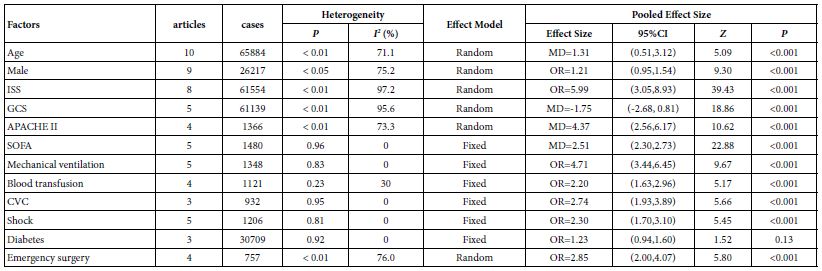
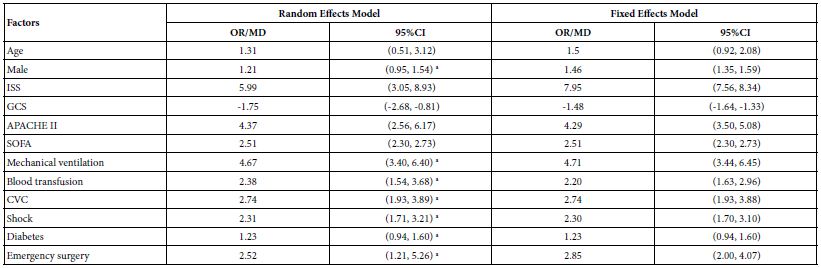
An analysis was conducted on the 12 included influencing factors. For SOFA, mechanical ventilation, number of blood transfusions, central venous catheterization, shock, and diabetes, the I² was ≤30, so a fixed-effects model was chosen for analysis. For the remaining factors, the I² was ≥50%, so a random-effects model was used. The study results indicated that, except for diabetes, all other factors were statistically significant (P<0.05) (Table 2).
Table 2: Meta-Analysis of Influencing Factors
Sensitivity Analysis
The pooled effect size and heterogeneity for the 12 influencing factors were estimated using both random-effects and fixed- effects models. The statistical results showed that, except for the ISS, the other influencing factors demonstrated good consistency, indicating a high level of reliability in the results of this study (Table 3).
Table 3: Sensitivity Analysis of Influencing Factors
Quality Evaluation and Publication Bias
The NOS scoring results showed that 7 articles scored ≥7 points [11,13-15,17-19] and 3 articles scored 6 points [12,16,20]. Quality evaluation is provided by Supplemental Table 2. Egger’s regression test was used to assess publication bias for the 10 articles that considered age as a risk factor for sepsis. The Egger’s regression test for funnel plot asymmetry supports this observation, yielding a non-significant result (p = 0.32), which indicates a low level of bias in the published findings. The contour-enhanced funnel plot as shown in Supplement Figure 1. For the other 11 influencing factors, the number of included articles did not reach 10, hence no publication bias analysis was conducted for them.
Discussion
The pooled average incidence of sepsis in adult trauma patients calculated from the studies was 35.2%, which is higher to the 31.1% reported by Amina Abliz et al. [21]. The estimation of incidence rates varies by region. This study found that the incidence rate in China is 60.1%, which is significantly higher than the 10.3% in other countries. The reason for this difference may be related to the data sources. Among the five foreign studies included, the data of three studies come from public databases. Such data sources may have a more representative sample of the general population, but issues such as data collection methods and quality control may lead to an underestimation of the incidence rate. In contrast, the data of the five domestic studies all come from hospitals, which means that the data mainly come from patients seeking medical treatment, and there may be selection bias. Hospital – based data tend to be biased towards patients with more severe or symptomatic conditions, which may overestimate the incidence rate. Furthermore, the decrease in the incidence of post – traumatic sepsis over time may be attributed to early diagnosis and intervention, continuous strengthening of hospital infection control measures, improvement of the trauma treatment system, and enhanced self – health awareness of patients after trauma. Finally, compared with previous standards, the Sepsis – 3 diagnostic criteria may have improved sensitivity. This comprehensive assessment method may lead to the diagnosis of more sepsis patients in early or sub – clinical states, thereby resulting in an increase in the incidence rate.
Advanced age is an important risk factor for sepsis in adult trauma patients. The elderly are more susceptible to sepsis due to factors such as immunosenescence, weakened cardiovascular function, poor nutritional status, and comorbidities [22]. Epidemiological studies have shown that the incidence of sepsis is higher in males than in females [23]. The results of this study indicate that the risk of sepsis in male trauma patients is 1.21 times higher than in females, which is close to the 1.3 times reported in a study from the United States [24]. This may be related to differences in sex hormone levels [25]. Although demographic-related influencing factors cannot be directly intervened, the development of sepsis in elderly male trauma patients should be closely monitored. Additionally, APACHE II and SOFA scores are used to assess the severity of patients’ conditions. The risk of sepsis is positively correlated with these scores. The lower the GCS score, the higher the risk of sepsis. Particularly, patients with severe brain injuries and coma have a higher incidence of sepsis and septic shock [26]. The ISS score provides a quantitative measure for assessing soft tissue injuries in trauma patients. This study found that ISS, APACHE II, SOFA, and GCS scores are all helpful for early identification of sepsis in adult trauma patients. Medical staff need to closely monitor patients with abnormal scores and take timely intervention strategies to prevent the occurrence of sepsis. Furthermore, the number of blood transfusions, mechanical ventilation, central venous catheterization, and emergency surgery are associated with an increased risk of sepsis in trauma patients. Blood transfusion may increase the risk of sepsis by suppressing immune responses [27]. Patients on mechanical ventilation are more likely to develop VAP, leading to sepsis [28]. Central venous catheterization increases the risk of central venous catheter-related bloodstream infections, especially in the intensive care unit, where such infections are common and potentially life- threatening [29]. Emergency surgery is also a risk factor for sepsis after trauma. The OR value of this study is 2.55, indicating that the risk of sepsis in patients undergoing emergency surgery is 2.55 times that of those undergoing elective surgery, which is close to the 2 times reported in previous studies [30].
Therefore, in the management of trauma patients, the necessity of blood transfusions, mechanical ventilation, central venous catheterization, and emergency surgery should be carefully assessed to reduce the risk of sepsis. Lastly, shock can predispose patients to sepsis by damaging microcirculation and reducing tissue perfusion, while sepsis can exacerbate shock by triggering widespread inflammatory responses and cardiovascular dysfunction [31]. Therefore, when trauma patients have shock, it should be promptly recognized and treated to reduce the incidence of sepsis.
Limitations
This meta-analysis has several limitations. Firstly, there is a certain degree of heterogeneity in the combined effect sizes of some risk factors, which may be related to factors such as the race, age distribution of the study subjects, and the quality of diagnosis and treatment in different medical institutions, and thus needs further improvement; Secondly, risk factors with less than 10 studies were not assessed for publication bias, so the possibility of bias cannot be ruled out. Moreover, the study did not categorize sepsis by severity, which could affect treatment strategies and outcome predictions.
Conclusion
In conclusion, the incidence of sepsis in adult trauma patients is high and influenced by various factors including age, gender, clinical scoring systems, invasive procedures, as well as comorbid conditions. Clinical medical staff can refer to the results of this study, deal with and prevent risk factors in a targeted manner, reduce the occurrence of sepsis, and thus improve the prognosis and quality of life of trauma patients.
CRediT Authorship Contribution Statement
Bingsheng Wang conceived and designed the study, independently completed database search. Wenhao Qi screening and data extraction and writing. Bing Wang, Xiaohong Zhu and Chaoqun Dong conducted statistical analysis, interpreted the analytical results, and provided technical support for methodological refinement. Yankai Shi, Jiani Yao and Xiajing Lou assisted in optimizing the research. Aili Shi and Shihua Cao reviewed and edited the manuscript.
Acknowledgements
This research was supported by the Medical and Health Technology Plan of Zhejiang Province (grant 2022507615); Key Research Project for Laboratory Work in Zhejiang Province Colleges, ZD202202; Zhejiang Province Traditional Chinese Medicine Inheritance and Innovation Project 2023ZX0950. 2024 research project of Engineering Research Center of Mobile Health Management System, Ministry of Education; First – class Undergraduate Course in Zhejiang Province, 2022, sponsored by the Education Department of Zhejiang Province (No.1133).
References
- Skelton JK, Purcell R (2021) Preclinical models for studying immune responses to traumatic injury. Immunology 162: 377-388. [crossref]
- Zeng L, Du J, Gu W, Zhang AQ, Wang HY, et (2015) Rs1800625 in the receptor for advanced glycation end products gene predisposes to sepsis and multiple organ dysfunction syndrome in patients with major trauma. Crit Care 19: 6. [crossref]
- M SH, Gs P, Ml L, Seymour CW, Liu VX, et (2016) Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315. [crossref]
- Sauaia A, Moore FA, Moore EE (2017) Postinjury Inflammation and Organ Crit Care Clin 33: 167-191. [crossref]
- Liang Huaping, Zhu Junyu, Hu Mingdong (2021) Several Key Issues in the Field of Traumatic Sepsis Chinese Journal of Traumatology 37: 385-389.
- Khan S (2020) Introduction to Meta-analysis. In: Khan S, ed. Meta-Analysis: Methods for Health and Experimental Studies. Statistics for Biology and Health. Springer 15-36.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372: n71. [crossref]
- Bahemia IA, Muganza A, Moore R, Sahid F, Menezes CN (2015) Microbiology and antibiotic resistance in severe burns patients: A 5 year review in an adult burns Burns 41: 1536-1542. [crossref]
- Stang A, Jonas S, Poole C (2018) Case study in major quotation errors: a critical commentary on the Newcastle-Ottawa scale. Eur J Epidemiol 33: 1025-1031. [crossref]
- Nakagawa S, Noble DWA, Senior AM, Lagisz M (2017) Meta-evaluation of meta- analysis: ten appraisal questions for BMC Biol 15: 18.
- Akaraborworn O, Chaiwat O, Chatmongkolchart S, et al. (2019) The intensive care unit admission predicting the factors of late complications in trauma patients: A prospective cohort Archives of Trauma Research 8: 203.
- Sun Shuying, Wen Dalin, Chen Guosheng (2023) Analysis on the Related Risk Factors for Sepsis in Patients with Severe Multiple Injuries and Their Early Warning Chinese Journal of Traumatology. Wound Pract Res 39: 443-449.
- Xu Jing, Jiao Xiaoqin, Guan Hong, Wang Pengsen, Du Junkai (2022) Mining on the Risk of Sepsis in Patients with Severe Journal of Clinical Emergency 23: 847- 853.
- Qi H, Yu S, Li L, Meng S, Chen T, et al. (2019) A new warning scoring system establishment for prediction of sepsis in patients with trauma in intensive care unit. Chinese Critical Care Medicine 31: 422-427. [crossref]
- Yu Yaofeng, Zhang Liqun (2018) Clinical Factor Analysis of Post-traumatic Infection Complicated with Sepsis in the Intensive Care Zhejiang Journal of Traumatic Surgery 23: 671-673.
- Gao Min, Sun Yu, Wang Yudi, Xia Wanqiu, Liang Huaping, et al. (2017) Risk Factor Analysis of Sepsis Complicated in Post-traumatic Infection Patients in the ICU. Acta Academiae Medicinae Militaris Tertiae 39: 367-372.
- Park JH, Choi SH, Yoon YH, Park SJ, Kim JY, et (2016) Risk factors for sepsis in Korean trauma patients. Eur J Trauma Emerg Surg 42: 453-458. [crossref]
- Wafaisade A, Lefering R, Bouillon B, et (2011) Epidemiology and risk factors of sepsis after multiple trauma: an analysis of 29,829 patients from the Trauma Registry of the German Society for Trauma Surgery. Crit Care Med 39: 621-628. [crossref]
- Plurad DS, Lustenberger T, Kilday P, Zhu J, Green DJ, et (2010) The association of race and survival from sepsis after injury. Am Surg 76: 43-47. [crossref]
- Osborn TM, Tracy JK, Dunne JR, Pasquale M, Napolitano LM (2004) Epidemiology of sepsis in patients with traumatic Crit Care Med 32: 2234-2240. [crossref]
- Amina Abulizi, Ahmatjan Pakhatin, Huang Yangmei, et (2021) Diagnostic Value of Biomarkers Combined with Trauma Scores for Post-traumatic Sepsis. Journal of Traumatic Surgery 23: 384-390.
- He W, Yao C, Wang K, Duan Z, Wang S, et al. (2024) Single-cell landscape of immunological responses in elderly patients with sepsis. Immun Ageing 21: 40.
- Lakbar I, Einav S, Lalevée N, Martin-Loeches I, Pastene B, et (2023) Interactions between Gender and Sepsis—Implications for the Future. Microorganisms 11: 746. [crossref]
- Martin GS, Mannino DM, Eaton S, Moss M (2003) The epidemiology of sepsis in the United States from 1979 through N Engl J Med 348: 1546-1554. [crossref]
- Min SY, Yong HJ, Kim D (2024) Sex or gender differences in treatment outcomes of sepsis and septic shock. Acute Crit Care 39: 207-213. [crossref]
- Lu HX, Du J, Wen DL, Sun JH, Chen MJ, et (2019) Development and validation of a novel predictive score for sepsis risk among trauma patients. World J Emerg Surg 14: 11. [crossref]
- Blajchman MA (2005) Transfusion immunomodulation or TRIM: what does it mean clinically? Hematology 10: 208-214. [crossref]
- Rubano JA, Paccione MF, Rutigliano DN, Vosswinkel JA, McCormack JE, et al. (2015) Outcomes following prolonged mechanical ventilation: analysis of a countywide trauma J Trauma Acute Care Surg 78: 289-294. [crossref]
- Pitiriga V, Bakalis J, Theodoridou K, Kanellopoulos P, Saroglou G, et (2022) Lower risk of bloodstream infections for peripherally inserted central catheters compared to central venous catheters in critically ill patients. Antimicrob Resist Infect Control 11: 137. [crossref]
- Moore LJ, Moore FA, Todd SR, Jones SL, Turner KL, Bass BL (2010) Sepsis in general surgery: the 2005-2007 national surgical quality improvement program Arch Surg 145: 695-700. [crossref]
- Gorecki G, Cochior D, Moldovan C, Rusu E (2021) Molecular mechanisms in septic shock (Review). Exp Ther Med 22: 1161. [crossref]