Abstract
Objective: To conduct a systematic review of the experiences of patients with Sjögren’s syndrome.
Methods: We performed a computerized search across PubMed, Web of Science, Embase, Cochrane Library, CINAHL, PsychINFO, Proquest, CNKI, CBM, Wanfang Data, and VIP databases to identify qualitative studies on the illness experiences of Sjögren’s syndrome patients from the inception of the libraries to September 2023. The JBI Critical Appraisal Tool for qualitative research in Australia was utilized to assess the quality of the included studies, and synthesis methods were employed to integrate the findings.
Results: Nine studies were included, yielding 32 findings that were categorized into 10 themes, culminating in 4 overarching outcomes: (1) prolonged and challenging diagnostic and treatment journeys; (2) significant daily life disruptions; (3) diverse coping styles and illness attitudes; (4) a pronounced need for, yet scarcity of, social support.
Conclusions: Sjögren’s syndrome patients endure profound physical and mental disturbances, leading to a markedly diminished quality of life. It is imperative for healthcare professionals to enhance symptom management and intervention, focus on assessing patients’ psychological well-being and coping mechanisms, and develop a comprehensive medical and social support system to ameliorate patients’ quality of life.
Keywords
Sjögren’s syndrome, Illness experience, Qualitative research, Meta-synthesis
Introduction
Sjögren’s syndrome (SS) is a chronic autoimmune disease hallmarked by dry mouth and eyes due to lymphocytic infiltration of the salivary and lacrimal glands, with primary clinical manifestations including xerostomia, fatigue, and musculoskeletal pain [1]. Predominantly affecting middle-aged and elderly women, the global incidence rate ranges from 0.04% to 4.80% [2]. SS is a protracted and relapsing condition; as it advances, symptoms can impact multiple bodily systems, severely compromising patients’ physical and mental health [3,4]. Amid the evolution of the bio-psycho-social medical model, the psychological well-being of patients with SS has become a focal point for researchers. Existing studies, while exploring the experiences and sentiments of SS patients, exhibit variations in racial, contextual, and methodological aspects, preventing a comprehensive understanding from a single study. This investigation employs a meta-integration approach to compile a more exhaustive qualitative evidence base reflecting the experiences of SS patients, aiming to inform clinical healthcare professionals and bolster the development of targeted interventions and measures.
Methods
The protocol was registered a priori with the International Prospective Register of Systematic Reviews (PROSPERO) under registration number CRD42023472699.
Search Strategy
PubMed, Web of Science, Embase, Cochrane Library, CINAHL, PsychINFO, Proquest, CNKI, CBM, Wanfang Data and VIP was searched for qualitative studies on the experience of SS from its inception to 30 September 2024, and the references of the included studies were searched manually. Search terms such as ‘Sjogren’s Syndrome/primary Sjogren’s syndrome/Sjogren’s syndrome/ Sicca Syndrome/Sicca exocrinopathy/SS/pSS; illness experience/ experience/feel*; qualitative research/qualitative research/qualitative study/participant observation/phenomenology/action research’ etc. The search strategy is illustrated with a PubMed example, see Figure 1.
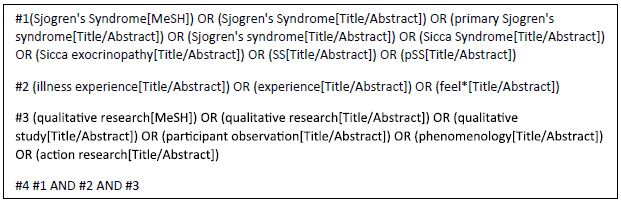
Figure 1: Pubmed search strategy
Literature Inclusion and Exclusion Criteria
The inclusion criteria referred to the PICoS model [5,6]. (1) Population (P): patients diagnosed with SS (including primary Sjögren’s syndrome and Sjögren’s syndrome), age≥18 years old, gender is not limited; (2)Interest phenomenon (I): patients with SS since the disease since the real experience of the disease and feelings; (3) Context (Co): the life experiences of patients with SS during or after the diagnosis and treatment process; (4)Study design (S): qualitative research, including phenomenology, Grounded theory, ethnography and action research. Exclusion criteria: (1)duplicated published literature; (3)non-Chinese and English literature; (2)literature with no access to full text.
Literature Screening and Data Extraction
Literature screening and data extraction were carried out independently by 2 researchers (1st and 2nd authors), with a 3rd researcher (4th author) assisting in judgement when differences of opinion were encountered. The retrieved literature was imported into Endnote21, duplicates were eliminated, titles and abstracts were read for initial screening, and the full text was further read for re-screening to make a final decision on whether to include the literature. The information extracted mainly included the author, year of publication, country, subject of study, research method, phenomenon of interest and findings.
Evaluation of Literature Quality
The included literature was evaluated by 2 researchers using the JBI qualitative research quality assessment tool [7]. The tool consists of 10 items designed to assess the quality of qualitative research literature with different methods, including research methodology and conceptual depth of information. 2 researchers were assessed with ‘yes’, ‘no’, ‘not clear’were used to assess the quality of the literature, which was classified into 3 grades, A, B, and C. All criteria were assessed as grade A if they were met, grade B if they were partially met, and grade C if none of them were met. Only studies with grades A and B were included in this study and studies with grade C were excluded. Disagreements, if any, were resolved through independent judgement by a 3rd researcher.
Meta Integration Methodology
The pooled integration method from the Australian JBI Centre for Evidence-Based Healthcare was employed to synthesize the qualitative research literature under review [7,8]. Researchers, well-versed in evidence-based nursing and experienced with qualitative methodologies, meticulously examined the included literature. This process aimed to comprehend and elucidate the significance of each finding, consolidate them into categories, and ultimately amalgamate these into novel insights by dissecting the interconnections between categories.
Results
Literature Search Results
The results of the initial literature search were 588 articles, and 9 articles were included after screening and quality evaluation. The time range was from 2001 to 2020, including 1 article in Chinese and 8 articles in English. Research methods phenomenology 6 articles, descriptive research 2 articles, grounded theory 1 article. The literature screening process is shown in Figure 2.
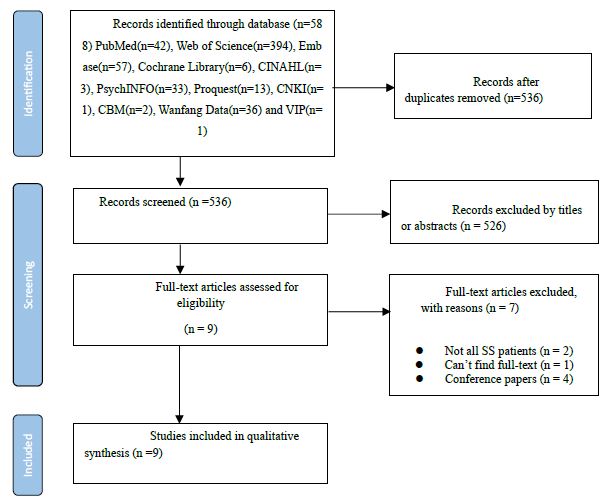
Figure 2: Flow chart of literature screening
Basic Characteristics and Quality Evaluation of the Included Literature
The basic characteristics of the literature are shown in Table 1 and the quality evaluation is shown in Table 2.
Table 1: The basic characteristics of the included literature(n=9).
|
Author |
Year | Country | Participants | Study design | Location | Aim |
Themes |
| Nancy et al. [9] |
2001 |
America | 10 patients | Descriptive Research | telephone interview | To explore the lived experiences of people with SS and to uncover the coping strategies and attitudes of actual patients with SS | Four themes: helping hindering hoping hurting |
| Rebecca J et al. [10] |
2017 |
The United Kingdom | 20 patients | Phenomenological Research | Hospital outpatient departments or research institutes | To investigate the experience of fatigue and related symptoms in patients with pSS | Three themes: the physical experience of fatigue; ocular fatigue and fatigue related to ocular complaints; cognitive aspects of fatigue |
| Jemma L et al. [11] |
2023 |
The United Kingdom | not mentioned | Phenomenological Research | Online Sites | To qualitatively explore the conversations about sexual functioning that females with SS had on internet forums | Four themes: the symptoms of SS and their impact on the sexual environment; the emotional responses that are commonly evoked in response to sexual difficulties; the strategies that users have implemented to manage sexual problems; and the impact that a partner’s behavior may have on the sexual environment. |
| Di Ying J et al. [12] |
2016 |
Singapore | 10 patients | Phenomenological Research | Dental school conference room | To provide clinicians with insight into how dry mouth can impact on the daily lives of Sjögren’s Syndrome patients | Four themes: the journey to diagnosis; disease impact spectrum (of dry mouth amid other symptoms); interactions with healthcare professionals; and the positive coping process. |
| Angelika et al. [13] |
2017 |
Austria | 20 patients | Phenomenological Research | Outpatient quiet room | To explore perspectives and needs of patients with PSS that influence health related quality of life (HRQL) | Three themes: Physical dimension; psychological & emotional challenges; social life & daily living |
| Gonzalo et al. [14] |
2016 |
Chile | 12 patients | Grounded Theory | Hospital lighting and soundproofed private rooms | To give an encompassing in-depth account of the life experiences of women with pSS and health-related behaviours, and to summarize these experiences in an integrated model. | Three themes: illness experience, social interaction and psychological response |
| Peng et al. [15] |
2023 |
Taiwan, Province of China | 14 patients | Phenomenological Research | Patient’s neighborhood fast food restaurant or hospital | To explore the experiences of SS patients seeking care | Four themes: annoying symptoms; difficulty in confirming a diagnosis; fear of medication side effects; confronting the disease |
| Anne et al. [16] |
2014 |
Norway | 9 patients | Phenomenological Research | not mentioned | To examine how fatigue may differ from ordinary tiredness in patients with primary Sjögren’s syndrome (SS) | Two themes: a heavy, resistant body and ever- present lack of vitality; unpredictable and uncontrollable fluctuations in fatigue |
| Kerry et al. [17] |
2020 |
The United Kingdom | 48 patients | Descriptive Research | Online Forum | To explore the disease and treatment experiences of patients with pSS | Three themes: Symptoms; Symptom Impacts; Patient Experiences with pSS Management |
Note: 1 Was there a clear statement of the aims of the research? 2 Is a qualitative methodology appropriate? 3 Was the research design appropriate to address the aims of the research? 4 Was the recruitment strategy appropriate to the aims of the research? 5 Was the data collected in a way that addressed the research issue? 6 Has the relationship between researcher and participants been adequately considered? 7 Have ethical issues been taken into consideration? 8 Was the data analysis sufficiently rigorous? 9Is there a clear statement of findings? 10 How valuable is the research?
Table 2: Methodological quality evaluation of the included literature (n=9).
|
Publication |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
10 |
| Nancy et al. [9] | Yes | Yes | No | No | Yes | No | Yes | Yes | Yes | Yes |
| Rebecca J et al. [10] | Yes | Yes | Yes | Unclear | Yes | No | Yes | Yes | Yes | Yes |
| Jemma L et al. [11] | Yes | Yes | Yes | Unclear | Yes | No | No | Yes | Yes | Yes |
| Di Ying J et al. [12] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Angelika et al. [13] | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes |
| Gonzalo et al. [14] | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Peng et al. [15] | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes |
| Anne et al. [16] | Yes | Yes | Yes | Unclear | Yes | No | No | Yes | Yes | Yes |
| Kerry et al. [17] | Unclear | Yes | Yes | Unclear | Yes | No | No | Yes | Yes | Yes |
Results of Meta-integration
The researcher distilled a total of 32 findings by iteratively reading and analyzing the nine pieces of literature included, organizing and generalizing the similar findings into 10 new categories, and obtaining four integrative findings.
Integrating Outcome 1: A Long and Difficult Consultation Experience
Category 1: Long Time to Diagnosis of Disease
Patients often experience multiple visits to the doctor due to disease symptoms involving multiple systems throughout the body (‘These searches were complicated by the need for multiple diagnoses including fibromyalgia, Raynaud’s, RA, lupus, and chronic fatigue syndrome’[9] ‘Many respondents discussed their histories of multiple doctor visits both to general practitioners and to specialists’[9]), in which most patients received only specialist symptomatic management (‘the focus of the physician’s visit was on prescribing medication to bring symptomatic relief ’[15]), and the time to confirmation of the diagnosis was continually prolonged (‘after 5 years of symptoms and unsatisfying visits at different doctors, one doctor was on the right way’[13]) they questioned the professionalism of the doctors (‘the thing is do the general practitioners know about it ?’[12] ‘Every practitioner speaks differently, three speak three ways and no one can tell me what it really is’[15] ‘My doctor doesn’t believe I have SS’[9])
Category 2: Difficult Treatment Process
Due to a lack of knowledge about the disease, patients often felt overwhelmed (‘she didn’t always know what was enough importance to alert her doctor’[9], ‘I don’t know that I actually really need to know all just at this point in time’[12]), and showed concern about medications that bring about side effects and effectiveness (‘worried about the side effects from western medication’[15], ‘the various medications do not help much’[9]), and financial burdens that grew as the disease progressed (‘every year thousands of dollars to the dentist’[12], ‘my retirement and savings have been depleted’[16])
Integration Outcome 2: Severe Daily Life Distress
Category 3: Physical Symptoms Throughout the Body
The most common discomfort experienced by patients is dry mouth and eyes (‘my lips stick together and I can’t separate them’[14], ‘my eyes are dry it feels like sandpaper has been rubbed over them’[16] ‘a feeling of choking’[13]), limited dietary choices (‘I can’t eat dry food, I can’t swallow it’[13]) Some patients experience a gradual loss of their sense of taste (‘sometimes I can’t taste food, I also find myself losing my sense of taste and smell’[14]); pain accompanies the patient (‘limbs, everything hurts’[13]), and constant fatigue fills the daily routine (‘just peeling potatoes is exhausting!’[15], ‘I don’t even have the energy to talk’[16], ‘I can sleep for days at a time when the fatigue comes’[10]), and sleep is affected (‘When I sit up in bed, I can only sleep’[13], ‘When I turn around, I have a feeling of suffocation’[13])
Category 4: Intimate Relationships in Trouble
Disease manifestations of oral dryness and female vaginal dryness (‘I don’t realise that I’m only comfortable with kisses on the mouth’[11], ‘My vaginal dryness has gotten worse’[11]) affect the patient’s intimate relationship harmony(‘My husband and I have not had sex for over a year’[11] ‘My husband does not tolerate changes in our sex life’)[14]), patients’ libido declines, intimacy decreases, and they feel guilt and pain (‘It’s too painful’[11] ‘The guilt overwhelms me’[11])
Category 5: Negative Psychological Experiences
Patients often feel helpless and sad in the face of the disease (‘especially when you are tired, you feel low’ [9] ‘one time I broke down and burst into tears, which stressed me out a lot’ [9]) SS is a chronic disease for which there is no cure for it, and a variety of symptomatic medications such as immunological agents and other drugs are mostly used in the clinic. While taking medications, patients are concerned about their potential range of side effects (‘anti-inflammatories, paracetamol, codeine, you end up with more tablets’ [11] ‘too many side effects of western medication’ [15]), and some patients are annoyed with the status (‘a few people questioned what they were doing to deserve SS’ [11], ‘I’m getting very, very annoyed’ [10] ‘I’m getting very, very bad’ [10]). During the course of the disease, the functioning of multiple organ organs throughout the patient’s body is progressively affected, and the patient expresses his or her fears about the uncertainty of the future progression of the disease (‘The worst thing is not knowing what is going to happen’ [8] ‘Fear of organ failure and dialysis’ [8] ‘fear of incapacitation’ [8]) In understanding the incurable nature of the disease, coupled with the constant physical and mental distress, patients develop self-loathing (‘I hate myself, I hate this woman in pain’ [10]), they chose to reject the sympathy of others and tried to hide the condition (‘don’t want people to look at me differently or say ‘poor me’’ [8] ‘I don’t let anyone see it…I cover everything up’ [9])
Category 6: Social and Work Disorders
SS symptoms affect all systems throughout the body and cause many inconveniences to the patient during daily life and social interaction (‘I can’t read at night because my eyes are too sore and tired’ [9] ‘Driving is often limited due to fatigue and dry eyes’ [8] ‘My tongue gets stuck and I can’t express myself clearly’ [13] ‘I have a very limited life of shutting myself away and going to the hospital’ [13]), and was unable to perform previous work (‘I have noticed that I get tired faster in conversations’ [9] ‘Especially with computer work, patients find it challenging to have long conversations with clients’ [12] ‘My dryness is greatly affected my life, causing me to stop working and retire early’ [16])
Integrating Outcome 3: Very Different Coping Styles and Attitudes Towards Illness
Category 7: Positive Attitude and Coping
Patient maintains a positive outlook throughout the disease diagnosis and treatment process, believing that he or she will ultimately overcome the disease (‘I’ll be lucky if that’s all that’s knocked out of me’ [8] ‘I think in time I’ll get back to where I was before’ [13] ‘There are a lot of people who lie down and die, they sink because of health problems – not me!’ [13] ‘I’m trying to say come across it and accept it’ [15]) They actively use multiple resources around them to seek help to learn about the disease (‘learning how to understand and help themselves from multiple sources such as other patients, support groups, literature and computer searches’ [8]) while attempting to make lifestyle adjustments to accommodate the disease (‘Many respondents drank water more frequently and changed their eating patterns. Keeping their hands and feet as warm as possible and pacing themselves according to their activity and rest needs’[8] ‘Made a lateral move to work’ [8] ‘We tried all the backwash.’[10] ‘My water bottle is my best friend’ [10] ‘Making vaginal uterine trays, moisturisers or soaps to alleviate the dryness associated with dry syndrome’ [10]), and some patients try alternative medicine treatments (‘Started actively exploring complementary and alternative medicine and started seeing a nutritionist’ [11]) Some patients comfort their souls by being religious and helping each other (‘I also attend spiritual events and worship God, all we do is ask for human nature’ [13] ‘We would go to church, and when we were sick we would ask our brothers and sisters in the group to pray for me, and then there would be an outlet for our moods’[15] ‘Doing small feats of charity myself, exhorting people to be good, teaching while doing so, and contributing my skills during my lifetime’[15]), and in doing so, patients experienced positive physical and mental positive feedback (‘personal growth and development can be facilitated’ [8] ‘the research process itself is an altruistic act that positively affects their self-esteem’ [11])
Category 8: Negative Attitudes and Coping Styles
Conversely some patients maintained negative attitudes and chose to delay seeking treatment (‘She tried to deny her symptoms and sometimes let the bad signs and symptoms go on for too long before seeking help’ [8] ‘She tried not to think about anything and took it day by day. I didn’t cope with it properly and that was my way’ [8]).
Integration Outcome 4: Thirst for and Lack of Social Support
Category 9: Lack of Social Support
SS patients do not receive sufficient support from family (especially spouses) and friends (‘My husband is the worst problem because he doesn’t understand’ [8] ‘My husband is not supportive or helpful, and doesn’t tolerate changes in our sex life’ ‘There are no friends to talk to about dry syndrome’ [8]) and on the other hand, the help received by patients in peer support groups is not sufficiently represented (‘There is a marked negativity in the support group and a lack of shared responsibility for managing the group’ [8] ‘The support group did not support her as a leader and she found herself dragged down by the others’ [8])
Category 10: Desire for Social Support
Adequate support from close relationships brought great help to the patient (‘More than one person said that her best support came from her spouse’ [8] ‘My whole family knows about this and they all try to help me not to talk too much and to keep me calm’[13]) Meanwhile, during the visit, patients were eager to be able to communicate effectively with each other and with healthcare professionals to give them psychological support and comfort (‘It’s very important to be able to talk to the healthcare professionals, I know that at the moment they can’t do anything about it, it’s okay, but you’re listening to it, you’re not just folding it’ [11] ‘An understanding healthcare practitioner made a big impact’ [8])
Discussion
Focus on the Impact of SS Symptoms on Patients and Actively Take Appropriate Measures to Alleviate Them
Integration results reveal that Sjögren’s syndrome (SS) patients endure a spectrum of symptoms, including dry mouth and eyes, fatigue, and generalized pain, significantly impairing their quality of life. As dry eyes can progress to keratitis, patients may experience blurred vision, redness, and ocular discomfort. Reduced salivary gland secretion not only affects eating and swallowing but also speech and taste perception, potentially leading to halitosis, oral ulcers, and rampant caries, which disrupt daily eating and social interactions [17- 18]. Healthcare professionals should advise patients on maintaining oral and ocular hygiene, facilitate early screening and diagnosis, and intervene to enhance glandular secretion, thereby mitigating the symptoms’ impact on physical and mental well-being. Sleep quality is closely linked to quality of life; sleep disorders can affect daily life and may trigger immune and inflammatory responses, increasing the risk of autoimmune diseases [19]. Professionals should assess and address patients’ sleep issues promptly, employing personalized treatments. Cognitive-behavioral therapy has been shown to improve sleep quality in SS patients, and both exercise therapy and traditional Chinese medicine (TCM) offer safe and effective interventions for sleep disorders [20,21]. Sexual dysfunction, a significant aspect of physical and mental health, is prevalent among female SS patients, threatening intimacy and potentially inducing negative emotions such as embarrassment and helplessness. Studies indicate that the prevalence of sexual dysfunction in SS patients is twice that of the general population, with vaginal dryness, pain, and fatigue influencing sexual behavior [22]. Given the sensitive nature of this issue, few patients are willing to discuss it openly. Healthcare professionals should delve into patients’ experiences, bolster nurse-patient trust, and provide empathetic listening, respect, and support. Collaborating with gynecologists and psychologists can offer patients comprehensive professional and psychological assistance.
There is no cure for SS, hence treatment focuses on symptom relief, mitigating local and systemic damage, and enhancing quality of life [23]. The emphasis should be on early screening and diagnosis through collaborative efforts with multidisciplinary teams. In recent years, traditional Chinese medicine (TCM) and its techniques have gained traction in SS treatment, attributed to their efficacy in symptom improvement and lower incidence of toxic side effects [24,25]. Future clinical outcomes may be enhanced by integrating TCM with other therapeutic approaches. Additionally, patients can be empowered to adopt healthier lifestyles, thereby improving their quality of life, through comprehensive and personalized health education initiatives.
Focusing on Negative Emotions in SS Patients and Fostering Positive Coping Strategies
Integrative findings reveal that SS patients experience a spectrum of negative emotions, impacting their quality of life due to enduring clinical symptoms, daily life limitations, and compromised social functioning [27]. Research indicates that the prevalence of anxiety and depression among SS patients is markedly higher than in the general population, with rates of 33.8% and 36.9%, respectively [26]. Healthcare professionals must prioritize the emotional well-being of SS patients, delve into the origins of their negative emotions, and guide them towards effective emotional expression and coping mechanisms. Encouraging a realistic understanding of disease symptoms and bolstering confidence in treatment outcomes is crucial. Evidence supports the efficacy of positive thinking training therapy and narrative care in alleviating anxiety and depression, thereby enhancing life quality [28-30]. Tailored interventions for SS patients can strengthen nurse-patient rapport, mitigate negative emotional impacts, and promote a positive and stable mental state.
The study’s findings highlight the diverse coping strategies employed by SS patients, which are their cognitive and behavioral responses to the disease and its associated disruptions [31]. Effective coping strategies are crucial for alleviating symptoms, enhancing functional status, and improving quality of life [32,33]. Healthcare professionals should promptly assess these strategies and provide ongoing support to patients who utilize positive approaches. Additionally, professionals must delve into the challenges faced by patients with negative or avoidant coping mechanisms to foster better disease acceptance and develop constructive cognitive coping strategies. Family support is pivotal in bolstering patients’ confidence in treatment and in converting negative emotions and coping behaviors [34]. Engaging patients and their caregivers in treatment decisions is essential for increasing their investment in therapy. Continuity of care, including regular professional guidance, is vital for encouraging patients to actively engage in their disease management and to confront their condition with a positive attitude.
Constructing an Optimal Medical and Social Support System
The integration findings indicate that Sjögren’s syndrome (SS) can affect multiple bodily systems, prompting patients to seek treatment for their presenting symptoms. Without adequate disease knowledge and interdisciplinary collaboration in diagnosis and treatment, healthcare providers may fail to make accurate assessments, leading to delayed SS diagnoses. During consultations, patients often receive only symptomatic treatment, which falls short of addressing their comprehensive needs. Thus, medical staff must enhance their expertise and foster interdisciplinary collaboration to develop personalized diagnostic and treatment plans, as well as offer patients thorough, evidence-based education and guidance on SS [23]. Patient care continuity should also be a priority, leveraging ‘Internet + nursing services’, interdisciplinary nursing teams, and hospital-community- family collaborative frameworks to ensure precise and efficient patient management [35]. Additionally, family, peer, and social support are crucial for SS treatment. Patients require ample emotional support from families, and peer support groups should be professionalized and made more effective. Group composition should be carefully selected to foster constructive communication and sharing among patients, with ongoing monitoring to address their emotional and informational needs, and to implement timely adjustments and management strategies.
Conclusion
Using meta-integration methodology, this study thoroughly examined the illness experiences of patients with SS, revealing four key themes: the complexity and duration of diagnostic and treatment processes, substantial disruptions to daily life, a variety of coping styles and illness attitudes, and an evident gap in social support despite a high demand. Healthcare professionals are advised to implement personalized care strategies to mitigate patients’ distressing symptoms, address psychological well-being to foster positive outlooks, and engage in interdisciplinary collaboration to enhance diagnostic and therapeutic approaches.
Limitation
This study has certain limitations: it did not include studies that have not yet been published, introducing a degree of selective bias; and some of the included literature is relatively old, which may limit the applicability of the meta-integrated results and may not fully reflect the experiences of SS patients. This indirectly suggests that there is a current lack of attention to the psychological experiences of SS patients, which warrants further in-depth exploration in the future.
Acknowledgements
We would like to express our sincere gratitude to all those who contributed to this work. Your support and assistance have been invaluable throughout the research process.
Conflicts of Interest
The authors declare no conflicts of interest.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
References
- Seror R, Nocturne G, Mariette X (2021) Current and future therapies for primary Sjögren syndrome. Nature Reviews. Rheumatology. [crossref]
- Cui Y, Li J, Li L, Zhao Q, Chen S, Xia L, Fu T, Ji J, Gu Z (2020) Prevalence, correlates, and impact of sleep disturbance in Chinese patients with primary Sjögren’s syndrome. International Journal of Rheumatic Diseases, 23(3): 367-373. [crossref]
- Zhang W, Li X M, Xu D, Liu D Z, Dong Y (2020) Recommendations of diagnosis and treatment of primary sjgren’s syndrome in china. Zhonghua nei ke za zhi. [Chinese journal of internal medicine], 59(4): 269-276. [crossref]
- Miyamoto, Samira T.Valim, ValeriaFisher, Benjamin A (2021) Health-related quality of life and costs in sjogren’s Rheumatology, 60(6) [crossref]
- Westerlund A, Kejs A M T, Beydogan H, Gairy K (2021) Primary Sjögren’s Syndrome: A Retrospective Cohort Study of Burden of Illness in Sweden. Rheumatology and Therapy. [crossref]
- Stern C, Jordan Z, McArthur A (2014) Developing the review question and inclusion The American Journal of Nursing. [crossref]
- The Joanna Briggs Critical appraisal checklist for qualitative research[EB/ OL].[2022-02-05].
- Lockwood C, Munn Z, Porritt K (2015) Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. International Journal of Evidence-based Healthcare. [crossref]
- Schoofs N (2001) Seeing the glass half full: living with Sjogren’s Journal of Professional Nursing: Official Journal of the American Association of Colleges of Nursing. [crossref]
- Stack R J, Southworth S, Fisher B A, Barone F, Buckley C D, Rauz S, Bowman S J (2017) A qualitative exploration of physical, mental and ocular fatigue in patients with primary Sjögren’s Syndrome. PloS One. [crossref]
- McCready J L, McCarty K, Deary V, Collins T L, Hackett K L (2023) A qualitative exploration of internet forum discussions surrounding female sexual function for individuals with Sjögren’s PloS One 18(9): e0291422.
- Ngo DYJ, Thomson WM, Nolan A, Ferguson S (2016) The lived experience of Sjögren’s BMC oral Health. [crossref]
- Lackner A, Ficjan A, Stradner MH, Hermann J, Unger J, Stamm T, Stummvoll G, Dür M, Graninger WB, Dejaco C (2017) It’s more than dryness and fatigue The patient perspective on health-related quality of life in Primary Sjögren’s Syndrome – A qualitative study. PloS One 12(2) e0172056. [crossref]
- Rojas-Alcayaga G, Herrera Ronda A, Espinoza Santander I, Bustos Reydet C, Ríos Erazo M, Wurmann P, Sabugo F, Geenen R (2016) Illness Experiences in Women with Oral Dryness as a Result of Sjögren’s Syndrome The Patient Point of View. Musculoskeletal Care 14(4): 233-242. [crossref]
- Chih-Yu P, Mei-Ping L, Pin-Hsuan L, Cheng-I Y, Huai-Ti H, Meng-Chen H, Li- Hung L (2023) Experiences of patients with Sjögren’s Syndrome in seeking medical Nursing Magazine 70(5): 36-43.
- Mengshoel AM, Norheim KB, Omdal R (2014) Primary Sjögren’s syndrome fatigue is an ever-present fluctuating and uncontrollable lack of energy. Arthritis Care & Research 66(8): 1227-1232. [crossref]
- Gairy K, Ruark K, Sinclair SM, Brandwood H, Nelsen L (2020) An Innovative Online Qualitative Study to Explore the Symptom Experience of Patients with Primary Sjögren’s Rheumatology and Therapy 7(3): 601-615. [crossref]
- Baer AN, Walitt B (2017) Sjögren Syndrome and Other Causes of Sicca in Older Clinics in Geriatric Medicine 33(1): 87-103. [crossref]
- Chung SW, Hur J, Ha YJ, Kang EH, Hyon JY, Lee HJ, Song YW, Lee YJ (2019) Impact of sleep quality on clinical features of primary Sjögren’s syndrome. The Korean Journal of Internal Medicine 34(5): 1154-1164. [crossref]
- Oláh C, Schwartz N, Denton C, Kardos Z, Putterman C, Szekanecz Z (2020) Cognitive dysfunction in autoimmune rheumatic diseases. Arthritis Research & Therapy 22(1) 78. [crossref]
- Chen HH, Lai JN, Yu MC, Chen CY, Hsieh YT, Hsu YF, Wei JC (2021) Traditional Chinese Medicine in Patients With Primary Sjogren’s Syndrome A Randomized Double-Blind Placebo-Controlled Clinical Trial. Frontiers in Medicine 8 744194. [crossref]
- Lp D, Aba G, Pa M et al. (2022) The effects of resistance training in patients with primary Sjögren’s Clinical Rheumatology 41(4) [crossref]
- H I, M I, O A et (2017) Are the women with Sjögren’s syndrome satisfied with their sexual activity?. Revista Brasileira de Reumatologia 57(3) [crossref]
- Liu H, Wang X, Liu W, He G, Liang X, Bian Y (2023) Effectiveness and Safety of Traditional Chinese Medicine in Treatment of Primary Sjögren’s Syndrome Patients A Meta-analysis. Combinatorial Chemistry & High Throughput Screening 26(14) 2554-2571. [crossref]
- Yen CM, Lin HC, Chen WS, Hsu CC, Liaw CC, Kung YY, Ma CP, Chen HY, Su YT, Chang CM (2024) Evaluation of traditional Chinese medicine tea bag TBDESJS in patients with Sjögren’s syndrome and dry eye syndrome A phase II pilot study. International Journal of Rheumatic Diseases 27(11) [crossref]
- Popescu A, Hickernell J, Paulson A, Aouhab Z (2024) Neurological and Psychiatric Clinical Manifestations of Sjögren Current Neurology and Neuroscience Reports 24(8): 293-301. [crossref]
- Cui Y, Xia L, Li L et (2018) Anxiety and depression in primary Sjögren’s syndrome A cross-sectional study. BMC Psychiatry 18(1): 131. [crossref]
- Liu Z, Dong Z, Liang X et (2017) Health-related quality of life and psychological status of women with primary Sjögren’s syndrome A cross-sectional study of 304 Chinese patients. Medicine 96(50) e9208. [crossref]
- Mao WJ, Chen WD, Cai WD, Jiang MJ, Du J, Guo JY (2024) Effects of virtual reality- based positive thinking training on negative emotions and fatigue in ovarian cancer patients undergoing chemotherapy. China Nursing Management 24(1): 29-34
- Lin Wan-Ting, Cai-Hong Lu, Zheng-Rong Wang, Huan Hong, Qiao-Rong Liu (2023) Effects of Focused Solution Brief Therapy Combined with Positive Thinking Training on Anxiety, Depression, and Quality of Life in Dry Eye Journal of Nursing 38(14): 72-76
- Zhao Jiao, Li Aixian, Feng Yuanyuan, Zhu Ying, Yuan Jiu-Lian, Xu Meng (2022) Effects of narrative care on anxiety, depression and well-being in hematopoietic stem cell transplantation patients. China Nursing Management.
- Folkman S (1984) Personal control and stress and coping processes A theoretical Journal of Personality and Social Psychology 46(4): 839-852.
- Líška D (2022) Exercise in the treatment of ankylosing Vnitrni Lekarstvi 68(E-1): 16-21. [crossref]
- Macfarlane TV, Abbood HM, Pathan E et al. (2018) Relationship between diet and ankylosing spondylitis A systematic European Journal of Rheumatology 5(1): 45-52. [crossref]
- Yang HL, Wang P, Hou WX, Luan XR (2016) Design and application of a hospital- community-family ternary linkage continuity of care platform. Chinese Journal of Nursing.