Abstract
Tissue engineering technology has demonstrated significant potential for tissue repair, enabling the restoration of damaged tissues or organs in terms of both structure and function. The utilization of digital light processing (DLP)-based 3D printing has gained significant traction in tissue repair due to its remarkable advantages in terms of printing resolution and efficiency, as well as mild printing conditions. Gelatin methacryloyl (GelMA) has emerged as a commonly utilized ink for DLP-based 3D printing due to its unique photoinduced crosslinking properties, controllable mechanical properties, degradation characteristics, and excellent biocompatibility. This paper primarily presents state-of-the-art technologies and applications involving DLP- based 3D printed GelMA constructs for bone repair, skin repair, and peripheral nerve repair. It aims to highlight the promising potential of DLP-based 3D printed GelMA constructs in regenerative medicine.
Keywords
Digital light processing, 3D printing, Gelatin methacryloyl, Tissue repair
Introduction
The repair and functional reconstruction of tissue and organ defects pose significant challenges in the field of regenerative medicine. Currently, autologous or heterologous tissue and organ transplantation are the most commonly used treatments; however, they are hindered by limitations such as traumatic trauma treatment, insufficient donor availability, and immune rejection. Tissue engineering research focuses on three core elements: cells, biomaterials, and tissue construction technology [1,2]. The realization of tissue and organ reconstruction relies on obtaining an adequate number of seed cells with specific biological activities, combining them with suitable biological scaffold materials, and employing precise construction techniques to create personalized physiological structures and functional organs or tissues in vitro. Therefore, personalized tissue engineering holds immense potential for advancements in the field of tissue repair and replacement. 3D printing technology offers rapid personalized manufacturing capabilities that can greatly contribute to tissue repair [3-5].Digital light processing (DLP)-based 3D printing utilizes a digital microscope device (DMD) to project images onto photosensitive liquid resin or bioink through surface exposure, enabling layer-by-layer solidification for printing purposes. DLP- based 3D printing technology enables the creation of personalized biological structures with precisely designable geometries, effectively bridging the structural disparities between engineered and natural tissues. It has found extensive applications in fabricating constructs such as artificial skin, bone implants, and nerve conduits. In comparison to other printing methods such as extruded and inkjet 3D printing, DLP-based 3D printing offers significant advantages in terms of resolution, efficiency, and working conditions. Its non-direct contact approach provides relatively gentle conditions for cell printing.
The development and application of printing ink is an important research connotation of dlp-based 3D printing technology. Conducting research and developing innovative bioinks that strike a balance between printability, biocompatibility, and mechanical performance is crucial for the advancement of bioprinting applications. GelMA, a photocrosslinkable hydrogel derived from gelatin modified with methacrylic anhydride, exhibits exceptional biocompatibility, visible light curing capabilities, and controllable mechanical properties, rendering it a versatile ink for printing purposes. During the printing process, GelMA is typically combined with cells, growth factors, and other bioactive substances to leverage 3D printing in fabricating tissue engineering models with specific structures and functionalities. This paper primarily presents state-of-the-art technologies and applications involving DLP-based 3D printed GelMA constructs for bone repair, skin repair, and peripheral nerve repair (Figure 1).
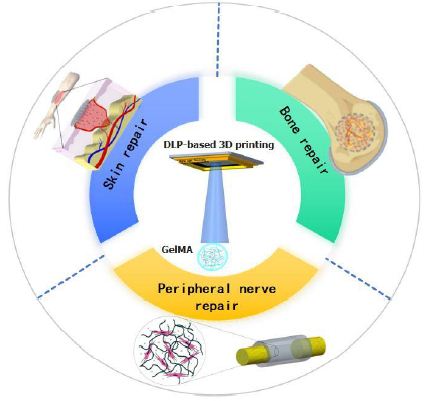
Figure 1: Application of DLP printing technology in tissue repair
DLP-Based 3D Printing
Based on the continuous application of DLP-based 3D printing in tissue engineering, higher printing accuracy and faster printing speed are required for practical implementation of DLP technology. Constant advancements in new printing technologies based on DLP technology are being made [6,7].
John et al. have designed a rapid continuous printing process based on DLP technology, which creates an oxygen-containing “dead zone” between the forming section and liquid precursors to enable continuous exposure printing and significantly enhance DLP printing speed [8]. Callum et al. have developed a dynamic interface printing technique based on DLP that utilizes sound modulation and restricted gas-liquid boundaries to generate centimeter-scale 3D structures within tens of seconds. This approach does not require complex feedback systems, specialized chemical reagents, or intricate optical elements while maintaining rapid printing speed and exhibiting immense potential for high-resolution and biocompatible applications {Vidler, 2024 #6}. Brett et al., on the other hand, have developed Computed Axial Lithographic (CAL) printing technology based on DLP where materials can achieve volumetric polymerization of arbitrary geometric shapes. Compared to traditional layer-by-layer printing methods, CAL’s polymerization approach eliminates the need for support structures, is suitable for high-viscosity fluids as well as solids, and significantly enhances print speed{Kelly, 2019 #4}. Regehly et al. employed dual-color photopolymerization in DLP-based 3D printing, wherein photoswitchable photoinitiators were developed. This technique utilizes two intersecting light beams of different wavelengths to achieve complete object fabrication by inducing localized polymerization within a confined monomer volume, resulting in enhanced speed and resolution for 3D printing. Recent advancements in DLP-based 3D printing have primarily focused on improving print speed, with various novel techniques offering additional technological approaches for bioprinting applications. In the realm of biological 3D printing technology, the choice of bioink plays a crucial role; currently, commonly utilized bioinks include alginate series bioinks, collagen bioinks, and GelMA materials [9]. CAL technologies introduce a printing paradigm shift because they are able to create entire objects at a time, rather than by adding basic building blocks in sequence. The study of Bernal et al. introduced the concept of volume bioprinting (VBP), which can manufacture an entire carrier cell structure of arbitrary size and structure in a time range of several seconds to tens of seconds. Using GelMA as printing material, bone scaffold and meniscus containing were constructed by volume printing technology. The rapid manufacturing advantage of CAL technology in bioprinting is verified [10].
GelMA
GelMA exhibits excellent biocompatibility and promotes cell adhesion and proliferation through its biological motifs, particularly the RGD sequences on gelatin molecules. The crosslinked network structure of GelMA not only serves as a scaffold for cells but also facilitates material exchange{Yue, 2015 #56} [11-13]. By adjusting the substitution degree of MA in GelMA, its mechanical properties such as viscosity, compressive strength, and tensile strength can be tailored to meet specific printing requirements. Additionally, for tissue repair applications, it is crucial that bioprinted structures are biodegradable. GelMA’s matrix metalloproteinase (MMP) site allows it to serve as an enzymatic degradation site recognized by injured organism cells [14]. As native cells fill the GelMA construct, they initiate its degradation while simultaneously repairing the area with their own cells to achieve tissue regeneration. With its exceptional biocompatibility, tunable mechanical properties, degradability, and photoinduced cross- linking capability, GelMA holds great potential for personalized and customized engineered living tissues or scaffolds for tissue repair [15- 18].
Applications of DLP-based 3D Printing Using GelMA
Tissue engineering aims to enhance or replace biological functions for the purpose of repairing damaged tissues and organs. DLP bioprinting enables precise distribution of cells, materials, and biological factors, offering a novel approach for fabricating artificial tissues. DLP-based 3D printing exhibits remarkable advantages in terms of resolution, efficiency, and operational conditions; moreover, its indirect contact formation method provides relatively mild conditions for cell printing. GelMA and its composite hydrogel system are exceptional biomaterials for tissue engineering due to their excellent biocompatibility, tunable mechanical properties, and degradability. The utilization of GelMA in DLP-based 3D printing holds great promise in various tissue repair applications including bone regeneration, skin reconstruction, as well as peripheral nerve restoration.
Bone Repair
The incidence of bone defects caused by trauma, infection, tumors, and congenital or metabolic diseases has significantly increased. These defects often result in functional disabilities and deformities, posing a clinical challenge for treatment. Traditional autologous and allogeneic bone transplantation methods have several limitations including inadequate tissue supply, donor site damage, immune rejection risks, and potential infections. Therefore, the development of new strategies for bone defect repair has become an urgent problem to be addressed [19]. On one hand, 3D printing enables personalized customization for individualized precision treatment; on the other hand, it reduces the cost associated with large-scale preparation [20]. The architecture of the bone repair scaffold can affect the effect of cell-induced regeneration of damaged bone. Song et al. combined bionic microporous GelMA/SilMA with hydroxyapatite (HAp) to prepare a bionic microporous GelMA/SilMA/HAp ink. By utilizing DLP-based 3D printing, they fabricated layered bionic microporous GelMA/SilMA/HAp (M-GSH) scaffolds. Animal experiments demonstrated that these bionic microporous scaffolds significantly enhanced tissue integration and bone regeneration after 12 weeks of implantation. Tissue engineering scaffolds for repair require not only adequate structural stability, but also good biocompatibility [21]. Gao et al. successfully developed GelMA/PEGDA/F127DA composite hydrogel scaffolds by DLP-based 3D printing, which not only facilitated cell adhesion and proliferation but also effectively promoted osteogenic differentiation of mesenchymal stem cells in osteogenic inductive environments. Intramembranous ossification and endochondral ossification are two ways of bone regeneration, in which hypoxia-inducing factor-1 α (HIF-1 α) signaling pathway can promote endochondral ossification and angiogenesis [22]. Gao et al. DLP-based 3D printing to fabricate structurally robust and biocompatible GelMA/PMAA hydrogel scaffolds, capable of chelating iron ions and continuously activating the hypoxia-inducible factor- 1α (HIF-1α) signaling pathway, thereby promoting endochondral ossification and angiogenesis processes as well as late-stage vascular formation and bone remodeling. The balance between cell survival environment and hydrogel cross-linking density is crucial for light sensitivity to achieve high intensity and good cell viability in cell- borne cartilage repair materials [23]. Shen et al., employing GelMA/ SG as bioink, created high-precision networked DLP printed scaffolds with superior shape retention compared to GelMA alone. In vitro experiments exhibited significant chondrocyte proliferation, while ectopic cartilage formation was evaluated by subcutaneously implanting the GelMA/SG scaffolds in nude mice. The utilization of these scaffold materials along with their manufacturing strategy offers potential solutions for future clinical challenges in cartilage repair. “Sr” is a potent anti-osteoporotic agent with anti-resorptive and anabolic properties, but with side effects when applying systemic administration. GelMA-SR doped nanosized hydroxyapatite (SrHA) composite hydrogel scaffold with controllable Sr delivery capability [24]. Cosmin et al. DLP-based 3D printing developed a novel GelMA- strontium-doped nanohydroxyapatite (SrHA) composite scaffold for bone tissue regeneration featuring controllable strontium (Sr) release capabilities. They investigated the biocompatibility of the composite hydrogel scaffold. In vitro cell culture demonstrated that osteoblasts could adhere and proliferate on the surface of the hydrogel. The DLP- prepared GelMA composite hydrogel tissue engineering scaffolds offer innovative avenues for research in bone loss repair [25].
Skin Repair
The prevalence of burn and skin ulcer patients is significant, with chronic skin ulcers having a severe impact on their quality of life. Therefore, there is a great need for the development of scaffolds or biomimetic skin through tissue engineering. By utilizing 3D printing techniques that combine human keratinocytes, fibroblasts, and endothelial cells, rapid preparation of vascularized microstructures and perfused skin grafts can be achieved. DLP-based 3D printing provides a rapid manufacturing method to curing human skin fibroblast (HSF) and human umbilical vein endothelial cell (HUVEC) hydrogel material to form biomimetic skin. Zhou et al. utilized a biomimetic bioink (GelMA/HA-NB/LAP) and DLP-based 3D printing to fabricate functional living skin (FLS). FLS possesses interconnected microchannels that facilitate cell migration, proliferation, and new tissue formation. By mimicking the physiological structure of natural skin, FLS promotes skin regeneration and neovascularization. The three-dimensional (3D) artificial skin model provides a variety of platforms for testing skin transplantation, disease mechanisms and skin tissue. However, achieving physiological complexes in such hierarchical structures, such as the neurovasculature with living cells, is extremely difficult [26]. Choi et al. DLP-based 3D printing printed a full-thickness skin model by employing methacryloyl-modified silk fibroin (SFMA) and GelMA, incorporating multiple cell types. They evaluated the printability, mechanical properties, and cell viability of SFMA/GelMA construct at various concentrations in order to determine the optimal printing concentration for artificial skin models. The simulation model confirmed that epidermal growth factor could enhance wound healing in both epidermal and dermal layers [27].
Peripheral Nerve Repair
Peripheral nerve injury is a significant cause of disability, often resulting in motor and sensory impairments. Treating peripheral nerve injuries poses a major technical challenge in the fields of reconstructive surgery and regenerative medicine. Utilizing DLP-based 3D printing, the rapid fabrication of personalized nerve conduit shows promise as an effective method to enhance peripheral nerve healing.The nerve conduit is a promising treatment for long-gap peripheral nerve injury, but with limited efficacy. Drug-releasable scaffolds may provide a reliable platform to construct a regenerative microenvironment for neural recovery. Tao et al. A functional nanoparticle-enhanced nerve conduit for promoting peripheral nerve regeneration was prepared by DLP-Based 3D Printing. The conduit consists of a gelatin-methylacryanyl (GelMA) hydrogel and drug-loaded poly (ethylene glycol) -poly (3-caprolactone) (MPEG-PCL) nanoparticles dispersed in the hydrogel matrix. Such nanoparticles in the conduit can release Hippo pathway inhibitors to promote nerve regeneration and functional recovery [28]. Zhang et al. fabricated a biodegradable self-adhesive bandage by utilizing a series of clickable functionalized monomers, including azide-modified gelatin methacryloyl and dibenzylcyclooctyne-modified GelMA. This bandage possesses the capability to envelop injured nerves and selectively release drugs for neural repair purposes. Through electrophysiological assessment and histological examination using a rat sciatic nerve transection model, it was confirmed that the drug-loaded self-adhesive bandage developed by Zhang et al. effectively promotes peripheral nerve regeneration and facilitates recovery [29]. Zhang et al. A double-branched GelMA neural conduit was constructed by DLP-based 3D printing .The efficacy of the double-branch nerve conduit was evaluated by the transfer of the rat tibial nerve to the peroneal nerve. The results of functional and histological evaluation showed that the double-branch nerve conduit could not only promote the regeneration and functional recovery of the peroneal nerve in the injury, but also retain the function of the donor nerve, demonstrating the potential application of this conduit in nerve transfer [30]. Wu et al. successfully employed continuous DLP printing to manufacture elastic hydrogel conduits encapsulating nanodrugs, utilizing GelMA/methacryloyl-modified silk fibroin (SFMA) composite hydrogels. This material exhibited favorable effects on cell adhesion, proliferation, and migration. Electrophysiological, morphological, and histological evaluations conducted through animal experiments demonstrated that the conduit effectively promoted axonal regeneration, myelin sheath regeneration, and functional recovery by providing an optimal microenvironment. Peripheral nerve injury is a common condition that often causes disability and poses challenges to the surgeon. Drug-releasable biomaterials provide a reliable tool for regulating the nerve healing-related neurorepair microenvironment. A self-adhesive bandage was designed to form parcels around the injured nerve to promote nerve regeneration and recovery [31].
Conclusion
DLP-based 3D printing technology offers significant advantages in resolution, efficiency, and working conditions. Its non-direct contact forming method provides relatively gentle conditions for cell printing, making it a promising construction technology for tissue engineering. GelMA composite hydrogels possess excellent biocompatibility, adjustable mechanical properties, and good formability, presenting enormous application prospects in tissue repair. By adjusting GelMA’s substitution rate and compositing with other materials, hydrogel systems can be prepared to meet different application requirements. However, prior to the clinical implementation of GelMA construct, it is imperative to address concerns such as standardizing GelMA synthesis methods and ensuring the safety of photoinitiators and hydrogel materials. Additionally, material properties should be expanded to meet more complex clinical demands such as controlled degradability of GelMA materials. For DLP printing technology and equipment to fully realize its personalized advantages in 3D printing applications like bedside printing technologies need further development.
References
- Zhang J, et al. (2022) Tissue Engineering Microtissue: Construction, Optimization, and Tissue Eng Part B Rev 28: 393-404. [crossref]
- Jiang W, Mei H, Zhao S (2021) Applications of 3D Bio-Printing in Tissue Engineering and J Biomed Nanotechnol 17: 989-1006.
- Zhu W, et (2016) 3D printing of functional biomaterials for tissue engineering. Curr Opin Biotechnol 40: 103-112.
- Randhawa A, et al. (2023) Recent Advances in 3D Printing of Photocurable Polymers: Types, Mechanism, and Tissue Engineering Application. Macromol Biosci 23: e2200278. [crossref]
- Pavan Kalyan BG, Kumar L (2022) 3D Printing: Applications in Tissue Engineering, Medical Devices, and Drug AAPS PharmSciTech 23: 92. [crossref]
- Nam J, Kim M (2024) Advances in materials and technologies for digital light processing 3D printing. Nano Converg 11: 45. [crossref]
- Gong J, et al. (2022) Digital light processing (DLP) in tissue engineering: from promise to reality, and perspectives. Biomed Mater 17: 6. [crossref]
- Tumbleston JR, et al. (2015) Additive manufacturing. Continuous liquid interface production of 3D objects. Science 347: 1349-52. [crossref]
- Regehly M, et (2020) Xolography for linear volumetric 3D printing. Nature 588: 620-624. [crossref]
- Bernal PN, et (2019) Volumetric Bioprinting of Complex Living-Tissue Constructs within Seconds. Adv Mater 31: e1904209. [crossref]
- Xiao S, et al. (2019) Gelatin Methacrylate (GelMA)-Based Hydrogels for Cell Transplantation: an Effective Strategy for Tissue Stem Cell Rev Rep 15: 664-679. [crossref]
- Liu T, et al. (2020) Applications of Gelatin Methacryloyl (GelMA) Hydrogels in Microfluidic Technique-Assisted Tissue Molecules 25: 22. [crossref]
- Bupphathong S, et (2022) Gelatin Methacrylate Hydrogel for Tissue Engineering Applications-A Review on Material Modifications. Pharmaceuticals (Basel) 15: 2. [crossref]
- Kurian AG, et al. (2022) Multifunctional GelMA platforms with nanomaterials for advanced tissue therapeutics. Bioact Mater 8: 267-295. [crossref]
- Sun M, et al. (2018) Synthesis and Properties of Gelatin Methacryloyl (GelMA) Hydrogels and Their Recent Applications in Load-Bearing Polymers (Basel) 10: 11. [crossref]
- Rajabi N, et (2021) Recent Advances on Bioprinted Gelatin Methacrylate-Based Hydrogels for Tissue Repair. Tissue Eng Part A 27: 679-702. [crossref]
- Klotz BJ, et al. (2016) Gelatin-Methacryloyl Hydrogels: Towards Biofabrication- Based Tissue Trends Biotechnol 34: 394-407.
- Chen S, et al. (2023) Structure and Properties of Gelatin Methacryloyl (GelMA) Synthesized in Different Reaction Biomacromolecules 24: 2928-2941. [crossref]
- Zhou B, et (2023) GelMA-based bioactive hydrogel scaffolds with multiple bone defect repair functions: therapeutic strategies and recent advances. Biomater Res 27: 86. [crossref]
- Feng Y, et al. (2021) Application of 3D Printing Technology in Bone Tissue Engineering: A Curr Drug Deliv 18: 847-861. [crossref]
- Song P, et (2024) DLP Fabrication of Multiple Hierarchical Biomimetic GelMA/ SilMA/HAp Scaffolds for Enhancing Bone Regeneration. Biomacromolecules 25: 1871-1886. [crossref]
- Gao J, et al. (2023) 3D-Printed GelMA/PEGDA/F127DA Scaffolds for Bone J Funct Biomater 14: 2. [crossref]
- Gao J, et al. (2023) DLP-printed GelMA-PMAA scaffold for bone regeneration through endochondral ossification. Int J Bioprint 9: 754. [crossref]
- Shen J, et al. (2024) 3D bioprinting by reinforced bioink based on photocurable interpenetrating networks for cartilage tissue Int J Biol Macromol 254: 127671. [crossref]
- Codrea CI, et al. (2024) 3D-Bioprinted Gelatin Methacryloyl-Strontium-Doped Hydroxyapatite Composite Hydrogels Scaffolds for Bone Tissue Regeneration. Polymers (Basel) 16: 13. [crossref]
- Zhou F, et al. (2020) Rapid printing of bio-inspired 3D tissue constructs for skin Biomaterials 258: 120287. [crossref]
- Choi KY, et (2023) A digital light processing 3D-printed artificial skin model and full-thickness wound models using silk fibroin bioink. Acta Biomater 164: 159-174.
- Tao J, et (2019) Rapid 3D printing of functional nanoparticle-enhanced conduits for effective nerve repair. Acta Biomater 90: 49-59.
- Zhang J, et al. (2020) A 3D-Printed Self-Adhesive Bandage with Drug Release for Peripheral Nerve Repair. Adv Sci (Weinh)7: 2002601. [crossref]
- Zhang J, et al. (2022) Nerve transfer with 3D-printed branch nerve conduits. Burns Trauma 10: tkac010. [crossref]
- Wu W, et (2023) 3D printed elastic hydrogel conduits with 7,8-dihydroxyflavone release for peripheral nerve repair. Mater Today Bio 20: 100652. [crossref]