DOI: 10.31038/MIP.2022334
Abstract
In the family Staphylococcaceae, Staphylococcus aureus is coagulase-positive, Gram-positive cocci. The bacteria are an opportunistic pathogen that frequently infects people without showing any symptoms. Although being mostly safe at these locations, it is possible for it to sometimes enter the body through skin breaches (such as abrasions, cuts, wounds, surgical incisions, or indwelling catheters) and injure both humans and animals. The ability of bacteria that cause foodborne poisoning to generate toxins after or during intoxication determines their pathogenesis. Staphylococcus aureus is one of the most common bacteria that cause these illnesses, and it is a major factor in gastroenteritis brought on by eating contaminated food. The ingestion of Staphylococcal enterotoxins produced in the food results in Staphylococcal food poisoning. The abrupt onset of nausea, vomiting, cramping in the abdomen and diarrhea are among its symptoms. Resistance to -lactam antibiotics and Vancomycin has mostly been attributed to plasmids and staphylococcal cassete chromosomes in particular. When bacteria are exposed to -lactam antibiotics, the extracellular enzyme -lactamase, which is encoded by blaZ, becomes active and confers penicillin resistance. The enzyme opens the -lactam ring by hydrolization to affect it. Globally as a result of the ongoing spread of bacterial strains that are resistant to antibiotics in the environment and the potential for food contamination, staphylococcal antimicrobial resistance is a serious issue for public health.
Keywords
Staphylococcus aureus, Antimicrobial susceptibility, Public health importance
Introduction
Staphylococcus aureus is a gram-positive, round (coccus) bacteria found in grape-like (staphylo) clusters; opportunistic colonies cause extreme harm. This bacterium is characterized by non-motile, non-spore forming and catalase positive which grow aerobically but which are capable to grow as facultative anaerobic [1]. Staphylococci are mostly occurs as harmless bacteria, that inhabiting the skin and soft tissue /nasal cavities of humans and animals. Among 31 species of staphylococci currently recognized, 15 are potentially pathogenic and It can causes a wide range of conditions in humans and animals, from mild skin infections to life-threatening bacteremia [2]. Staphylococcus aureus can also causes abscess in deep organs, by producing a toxin mediated diseases, self-limiting skin infections to life-threatening pneumonia, catheter-associated bacteremia, osteomyelitis, endocarditis, septicemia, Foodborne-illness and toxic shock syndrome (TSS) among other infections [3,4]. Meat is one of the animal product origins that contains high source of protein and vitamins for human being, again meat has high water content and rich in minerals and other nutrients which are suitable for the development of microorganisms. Due to its chemical composition and biological characteristics, meats are highly perishable foods providing a good source of nutrients for the growth of different microbial, that can leads infection in humans and also can lead to economic loss due to spoilage [5].
Staphylococcal food intoxication is happen due to the consumption of staphylococcal enterotoxins that preformed in the food. The main clinical manifestation of Staphylococcal food poisoning is vomiting, sudden onset of nausea, abdominal cramps and diarrhea. This condition is common in developing countries, because poor hygienic practices and low level of awareness. The staphylococcal enterotoxins are highly heat stable and are thought to be more heat resistant in food stuffs than in a laboratory culture medium. Due to this reason, even though we heating at normal cooking temperature, the bacteria may be killed but the toxins remain active. About half strains of staphylococcal strain are able to produce enterotoxins associated with food poisoning. Because of this condition enterotoxins producing Staphylococcus aureus are most dangerous and harmful for the human health [6]. Currently, Antimicrobial resistance is one of the most challenging situations to public health across the world. Even if different antimicrobial drugs are produced to treat S. aureus infections, the emergence and spread of antimicrobial resistant S. aureus can challenged for world to effectively treating and controlling of these. This is due to the high resistance percent could be traced to underuse or overuse of antibiotics due to poverty and ignorance, self-prescription, inappropriate prescription by physicians due to lack of effective antibiotic policies in our hospitals and other factors [7].
Staphylococci is one the most drug resistant bacteria, that develops resistance quickly and successfully to antimicrobial. This ways of defensive mechanism is due to consequence of the acquisition and transfer of antibiotic resistance plasmids and the possession of intrinsic resistance mechanisms [8] Currently, Methicillin-resistant Staphylococcus aureus (MRSA) strains are emerging wide spread to worldwide. Resistance to methicillin is mediated by different genes like, mec operon which is a part of the staphylococcal cassette chromosome mec (SCCmec). The mecA gene codes for an altered penicillin-binding protein, PBP2a, which has a minimum affinity for binding β-lactam antibiotics. The virulence of S. aureus was increased with existence of antibiotics resistance strains like Methicillin resistant S. aureus (MRSA) and Vancomycin resistance S. aureus [9].
Antibiotic resistance remains a major challenge in human and animal health. Resistance is increasingly being recognized in pathogens isolated from food. Food contamination with antibiotic-resistant bacteria can therefore be a major threat to public health, as the antibiotic resistance determinants can be transferred to other bacteria of human clinical significance. Furthermore, transfer of these resistant bacteria to humans has significant public health implications by increasing the number of food-borne illnesses and the potential for treatment failure. Food of animal origin could be contaminated from the farm, a situation which may be further compounded if the food is not properly handled during slaughtering and processing giving way for pathogens to multiply. Studies conducted in different countries to investigate the microbiological quality of food of animal origin reported the presence of potential human pathogens [10]. In general, S. aureus is one of the most common microbial, which causes diseases in both human and animals. Misuse of antibiotics in Livestock sector, Agriculture and in the treatment of human diseases, has contributed to the increase number of bacteria that are resistant to antimicrobial agents. Therefore, the main objective of this paper is to review the antimicrobial resistance in S. aureus from raw meat, virulence factors and focusing on the association between these characteristics and their implications for public and animal health.
Literature Review
Background of Staphylococcus aureus
Staphylococci family was first identified and isolated from the pus of surgical abscesses by the Scottish surgeon Sir Alexander Ogston in 1880 and he observed grape-like structure with circular in shape and he describe it staphylococcus. In 1881, Ogston found out that non-virulent staphylococci are also present on skin surfaces. Most staphylococcal strains from pyogenic lesions can produce golden yellow colonies, and the strains from normal skin, white colonies on solid media. In 1884, Friedrich Rosenbach name them Staphylococcus aureus (S. aureus) and S. albus respectively. Based on their characteristics and categorized them based on the production colonies color or pigments either golden or yellowish colonies. Later S. albus was renamed as S. epidermidis which were coagulase negative, mannitol non-fermenting and usually nonpathogenic strains.
The presence of Mobile genetic elements like bacteriophages, pathogenicity islands, plasmids, transposons, and staphylococcal cassette chromosomes enabled S. aureus to continually evolve and gain new traits. The genetic variation within the S. aureus species is approximately 22% of the S. aureus genome is non-coding and differ bacterium to bacterium, this is due to its reliance on heterogeneous infections. The different strains can secrete different enzymes/bring different antibiotic resistances to the group, increasing its pathogenic ability (https://en.wikipedia.org, 2021a).
Microbial Nomenclature
Staphylococcus aureus is a Gram-positive bacterium, which affects soft tissue and skin of host cell. The most common species of this pathogen that affects animal and human include S. aureus, S. intermedius, S. delphini, S. hyicus, S. schleiferi subsp. coagulans, S. pseudintermedius, S. equorum, S. xylosus, S. carnosus, S. simulans, S. saprophyticus, S. succinus, S. warneri, S. vitulinus, S. pasteuri, S. epidermidis, and S. lentus. One of these different species is S. aureus; so-named because of the color of the pigmented colonies (“aureus” means golden in Latin). Generally, S. aureus are opportunistic pathogens or commensals on host skin. However, they may act as pathogens if they gain entry into the host tissue through a trauma to the cutaneous barrier, inoculation by needles, the implantation of medical devices, or in cases in which the microbial community is disturbed or in immune compromised individuals [11,12].
Morphological and Biochemical Characteristics of Staphylococcus aureus
Morphologically, Staphylococcus aureus are characterized by spherical in shapes and after applying gram staining techniques, when examined under light electron microscope this bacteria can appeared as clusters resembling bunch of grapes with large round, golden-yellow colonies, often with hemolysis on blood agar Medias [13]. Additionally, S. aureus can produce an enzyme called coagulase. This enzyme reacts in the blood and produces a chemical called staphylothrombin. Staphylothrombin might make S. aureus even more difficult to kill by adding a layer of clotted protein to the bacterium membrane. Furthermore the S. aureus has a peptidoglycan membrane layer that would make it very hard for a bactericide drug to enter the cell and destroy it [14]. Biochemical test was one of the techniques that used to identify and differentiate S. aureus from other gram positive cocci microorganisms. Based on biochemical test, S. aureus is characterized by catalase-positive, which can be used to differentiate it from catalase-negative streptococci species and oxidase-negative. Staphylococci species can also be classified biochemically, S. aureus, which is coagulase-positive, produces a coagulase enzyme that agglutinates/clots blood or plasma while other medically important species of staphylococci, such as S. epidermidis and S. saprophyticus, are coagulase-negative. S. aureus can be distinguished from S. saprophyticus by novambicin susceptibility, while S. saprophyticus is novambicin-resistant.
Epidemiology of the Staphylococcus aureus
Staphylococcus aureus infections are found on the skin and mucous membranes. Human are the main reservoir for these organisms. Mostly, the S. aureus colonization up to 80% is common in health care workers, diabetics’ patient and intravenous drug users, hospitalized patients, and immunocompromised individuals [15]. The epidemiology of MRSA in particular has increased and distributed over the entire world. In general there are types of MRSA, this include community-associated MRSA, hospital-associated (HA-MRSA) and livestock-associated MRSA. Hospital-associated MRSA, the rise of novel strains of MRSA in the 1990s outside of the nosocomial environment will makes this pathogen to the recognition of “community-associated MRSA” (CA-MRSA), when compared to ancient hospital-associated (HA-MRSA) strains. In the mid-2000s, a third genre of MRSA was recognized, as colonization and infection of livestock and livestock workers and nominates it as livestock-associated MRSA (LA-MRSA) [16].
Distribution of S. aureus in Humans, Animals and Food of Animal Origin
Staphylococcus aureus is bacteria that normally reside in or on humans and does not usually cause infection. In 2019, Minnesota Department of health report on Staphylococcus aureus infectious disease, it stated that over 20% of their population almost always be colonized with S. aureus, while 60% of the population will be colonized with S. aureus either affected or not and the rest 20% are almost never colonized with S. aureus [17].
Meat is important food stuff and one of the main sources of protein, fats, minerals and vitamins. Meat contains high amount of water content and due to this reason most microorganism can growth easily, which leads to the food spoilage and foodborne infections to humans [18,19]. There are different mechanisms or factors that can initiate the growth of microorganism in meat. This factor includes; intrinsic factor and extrinsic (environmental factors), but the most common and efficient factors that contributes microbial to growth on meat are includes: – The temperatures in which meat can be storage, humidity and oxygen are the most important factors for microbial growth. Additionally, meat can be contaminated by these bacteria from the skin of animal during slaughtering at the abattoir and from different materials or equipment that are used for operation [20]. Currently, one of the most challenging problems in the world content is antibiotics resistance strains of S. aureus which pose a great risk in the food stuff. Of this meat of animal origin is one the most common sites at which drug residues can accumulate for a long period of time. Human being can gate this infection by eating contaminated meat [21-23]. Poor hygienic condition can cause meat to be contaminated by Staphylococcus aureus. When meat can contaminate by S. aureus; it can produce a toxin that activates disease. Even though, cooking destroys this pathogen, it will not destroy the toxin that produced by this pathogen, this is due to S. aureus can produce heat stable toxin [24]. Normally, S. aureus does not compete sufficiently with common microbial in raw foods; the contamination of food stuff with this pathogen is mostly associated with improper handling of foods, keeping of the food at which favorable for the growth of microorganism, which leads to multiplication of S. aureus and production of the enterotoxin [25].
Reservoirs and Sources of Infections
The primary ecological reservoir of Staphylococcus aureus causing infection in humans is the human nose, but a normal micro flora of the skin, hair, and mucous membranes may also be colonized. This pathogen can cause dermal infection if the cutaneous barrier is damaged. Any individuals that have been colonised by the bacteria are susceptible to any secondary infections, especially immune compromised people due to disease like HIV, type 1 diabetes and intravenous drug users, and patients undergoing hemodialysis, surgical patients are the most susceptible group for secondary infection. Additionally multiple sites in the body like, perineum, axillae, vagina, and gastrointestinal tract also were found to harbor this bacterium. Staphylococcus aureus in general have a commensal relationship with its host. The pathogen can causes disease in host tissue, when the skin of the host tissue can be damaged, inoculation by syringes, or by direct implantation with medical devices and leads infection in the host tissue. The main reservoirs of Staphylococcus aureus are infected mammary glands, ducts, and papillary lesions [26]. The primary reservoirs of S. aureus in affected countries are those animals in intensive systems like pigs, veal calves and broilers [27]. Normally S. aureus can be found in healthy cows, as carriers on the teat skin, nasal cavity, and rectum. But, the main reservoirs in a dairy cow are infected udders and teat skin [28]. From animal Pork is the main source of S. aureus reservoir host and human can gate this pathogen through consuming of the meat and causes foodborne illnesses. Staphylococcal foodborne infection is food poisoning disease that can occurs when human consume contaminated meat and the pathogen can induce staphylococcal enterotoxins expressed by enterotoxigenic strains of Staphylococcus species [29] S. aureus is an opportunistic pathogen that has capable to colonize a wide variety of host species, including birds and fish [30].
Modes of Transmission
Staphylococcus is the most common bacteria that cause mastitis in ruminants. The pathogen spread from one teat to another through the lining of the tea cups, milker’s hands, towels and fruit flies [31]. Staphylococcus including MRSA can be transmitted from animals to humans through direct contact especially from meat and also humans act as a reservoir for the transmission of S. aureus to vertebrate animals. Infections that can be present in both humans and animals and transmitted in both directions, such as S. aureus infections called as “amphixenoses. Different researcher can reported animal-to-human transmission of S. aureus in dairy sheep. S. aureus is usually transmitted by direct contact with colonised skin. Generally, Staphylococci can be transmitting from one species to another species or within the same species through direct or indirect contact with a patient who has a clinical infection of the respiratory or urinary tract and who is colonised with the bacterium. Contaminated surfaces and medical equipment are also used as a vehicle for transmission of MRSA (www.health.vic.gov.au).
Pathogenicity of Staphylococcus aureus
Virulence Factors
S. aureus possess different potential virulence factors that causes tissue damage: surface proteins that promote colonization of host tissues; invasions that promote bacterial spread in tissues (leukocidin, kinases, hyaluronidase); surface factors that inhibit phagocytic engulfment (capsule, Protein A); immunological disguises (Protein A, coagulase); membrane-damaging toxins that lyse eucaryotic cell membranes (hemolysins, leukotoxin, leukocidin and exotoxins that damage host tissues and leads disease [32]. S. aureus exotoxins, alpha-toxin, beta-toxin, delta-toxin and phenol soluble modulins are the cellular by products that activates the lysis of leukocytes (white blood cell), although α-toxin and phenol soluble modulins (PSMs) can also induces the formation of biofilms. Another surface-associated virulence factors like, protein A, fibronectin-binding antigen, and envelope associated proteins used to attaches and entrance of S. aureus to epithelial cells and initiates infection in the host cells [33]. S. aureus bacterial structures such as capsules, adhesins, extracellular products (enzymes) and toxins such as toxin α toxin β toxin leucocidin, enterotoxin, exfoliative toxin, and toxic shock syndrome toxin, contribute to different stages of infection [34]. Alpha toxin (α) is one of the vital virulence factors of S. aureus, that contains beta sheets which is water-soluble monomer targeting the red blood cells [35].
The formation of biofilms makes the pathogen to enter or live from the host cell, increasing their population within the host cell and protects the pathogen from environmental attack within the host cell. Enterotoxin is one of the dangerous toxins that mostly detect in the meat of animal origin due to S. aureus contamination and leads to gastroenteritis. S. aureus enterotoxin intoxication on consumers occurs through the establishment of contamination on food consumed. This enterotoxin is resistant to heat (heat stable), acid-resistant, and resistant to the effects of proteolytic enzymes like pepsin and trypsin [36]. Additionally biofilm formation is used the pathogen to attach to a living or non-living surface area which is used for grow and secrete several small molecules that attaches the microbial cells together [37]. Biofilms can cause antibiotics resistance, chronic disease and makes the host immune weak, because of it allows the pathogen to evade multiple clearance mechanisms [38]. S. aureus have capability to regulate the expression of virulence factors because of they have accessory regulatory gene (Agr) and the sigma factor (σB) and also this pathogen have ability adapt different microenvironments with environmental conditions, due to they generate the acquisition of genes like, bacteriophage, the staphylokinase gene and Panton-Valentine [39].
Mechanism of Disease Development
Although S. aureus is a normal flora of the skin and mucous membranes, any break in the skin or colonization of individuals with compromised immune systems can give an opportunity for this bacterium to invade and cause infection. The disease process can be mediated via two possible mechanisms; the production of toxins and the colonization that causes tissue invasion and destruction [40]. The pathogenicity of S. aureus is depends on the virulence factors that promote adhesion and evasion of the host immunologic responses. This organism can produce some toxins, that are causes diseases and a high mortality rate, of them toxic shock syndrome toxin (TSST) and Panton–Valentine leukocidin toxin, which causes necrotizing pneumonia and inducing leukocytosis and tissue necrosis [41]. Staphylococcus aureus can produce different kinds of virulence, which make to decrease in host’s immune system and causes diseases. Among S. aureus these virulence cytotoxins, nucleases, proteases, lipases, hyaluronidase, catalase, coagulase, collagenase, leucocidin, Toxic Shock syndrome (TSST-1), enterotoxins and exfoliative toxins are the most common virulence factors that S. aureus can produce in order to affect the host tissues. Other virulence factors are: – peptidoglycan, protein A, adhesion factors, teichoic acids, capsular polysaccharides and biofilms are the structural components that produce different toxin in the host cell (Figure 1) [42,43].
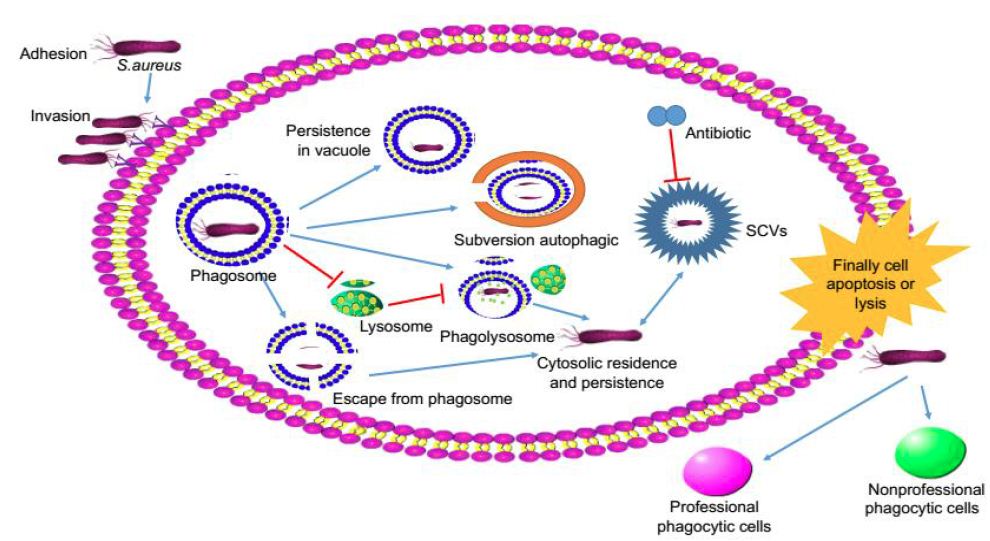
Figure 1: The mechanism of Staphylococcus aureus infection cells (Zhou et al., 2018)
The mechanism of Staphylococcus aureus disease development has five stages; this includes colonization, localization, dissemination and metastatic infections. The colonization proceeds to infection under certain predisposing factors such as prolonged hospitalization, immune suppression, surgeries, use of invasive medical devices and chronic metabolic diseases. Localized skin abscess develop when the organism is inoculated into the skin from a site of carriage. This can further spread and results in various clinical manifestations of localized infections such as carbuncle, cellulitis, and wound infection. The organism can enter into blood and spread systemically to different organs causing sepsis [44].
Disease Caused by Staphylococcus aureus
S. aureus was a bacterial infection that affects humans and all warm blooded animals. These organisms are the causative agents of different human and animal diseases, like bacteremia, endocarditis, impetigo, folliculitis, furuncles, carbuncles, cellulitis, scalded skin syndrome, osteomyelitis, septic arthritis, prosthetic device infections, pulmonary infections, and gastroenteritis, meningitis, toxic shock syndrome, and urinary tract infections.
Disease in Humans
Staphylococcus aureus causes a different form of disease in humans. Human staphylococcal infections are frequent, but usually remain localized at the portal of entry by the normal host defenses and leads to superficial lesions such as inflammation (characterized by an elevated temperature at the site, swelling, the accumulation of pus, and necrosis of tissue). Around the inflamed area, the fibrin will clot and the bacteria will form abscess. Additional this pathogen can causes Localized infection of the bone, which is called osteomyelitis and at serious stages it will causes septicemia and bacteremia, when the bacteria invade the blood stream. Moreover, S. aureus can causes more serious infections like pneumonia, mastitis, phlebitis, meningitis, and urinary tract infections; osteomyelitis and endocarditis. S. aureus is a major cause of hospital acquired (nosocomial) infection of surgical wounds and infections associated with indwelling medical devices. S. aureus causes food poisoning by releasing enterotoxins into food, and toxic shock syndrome [45].
Staphylococcus aureus is the leading cause of bacterial disease that harboring the health of human being and it causes gastrointestinal, respiratory, skin and soft tissue, and blood stream infections. In human S. aureus can causes different diseases ranging from ranges from mild stage to life threatening issues and hence most common is the skin infections which are often caused by abscesses. The most common disease of S. aureus on human are includes: purulent skin infections such as boils, abscesses, impetigo and scalded skin syndrome, systemic infections such as bloodstream infections, pneumonia, osteomyelitis, endocarditis and deep abscesses, hospital-acquired (nosocomial) infection of surgical wounds or treatment lines, infections of prosthetic devices such as pacemakers, heart valves, joint replacements and other foreign bodies, including central venous catheters and peritoneal dialysis catheters and food poisoning by releasing toxins into food toxic shock syndrome by releasing toxins into the bloodstream. Occasionally, staphylococcal infections can cause disease condition such as Bloodstream infections, Endocarditis, Osteomyelitis and Lung Infection.
Disease in Animals
S. aureus infections in animals are the most common reported as a cause of abscesses, mastitis, pneumonia and meningitis. Additionally, this pathogen can cause Abortion and stillbirth in sheep and goat [46]. In dairy cow, S. aureus causes mastitis. S. aureus can cause both acute and chronic form of mastitis. Acute form of mastitis caused by S. aureus is characterized by severe clinical infection with visible changes to milk color. The second typical sign of S. aureus in dairy cow is chronic form of mastitis, which is characterized by subclinical and under this condition there is no any change of milk color [47]. Staphylococcus aureus is the leading pathogen causing the most dangerous mastitis in cattle and the most difficult dairy product in most countries. Staphylococcus aureus has emerged as superbug of dairy udder, compromising animal health and economy. Its virulence is due to its ability of producing wide array of virulence factors that enhances its attachment, colonization, longer persistence and escaping the immune response. S. aureus can causes different disease conditions in pigs with starts from skin infections to severe condition. The most common infection caused by S. aureus in pig includes, septicemia, mastitis, vaginitis, metritis, osteomyelitis, and endocarditi. In small ruminants, S. aureus is a major cause of mastitis and septicemia. In goats, staphylococcal infection can allows the secondary infection because of the host immunity was decreased due to S. aureus infection and among the secondary infection that affects shoat due to this pathogen was Para poxvirus infection, which causes chorioptic mange or contagious pustular dermatitis. Staphylococcus aureus was also affect pet animal like dog and it causes different types of disease condition including pyoderma, otitis media, and wound infections [48].
Prevalence of Staphylococcus aureus from Meat
Globally, the prevalence of S. aureus ranges from 23.3% to 73 and the prevalence rate of S. aureus in raw meat in African countries are 16.0% in Tunisia, 57.8% in Ethiopia and 52.0% in Egypt were reported (Table 1) [49].
Table 1: Prevalence of Staphylococcus aureus from meat in the world
| Countries | Prevalence | Reference |
| Iran | 26.31% | Dehkordi et al., 2017 |
| United state | 27.8% | Carrel et al., 2017 |
| Colombia | 6% | Gutierrez et al., 2017 |
| China | 20.5% | Li et al., 2019 |
| Africa | 24.5%, | Thwala et al., 2021 |
| Chile | 47.6% | Valeria et al., 2019 |
| Indonesia | 58.3% | Wardhana et al., 2021 |
Prevalence of Staphylococcus aureus from Meat in the World
The prevalence of S. aureus in raw meat from different countries is varies, this is due to different reason like: – techniques of sample collection, season of the study, microbiologically examination methods, and meat handling methods [50]. In European countries, prevalence of Livestock Associated -MRSA ranging from 0 to 16% in broiler chickens, while the prevalence of chicken retail meat products ranges from 0 to 37% have been recorded. In general, the prevalence of Livestock Associated -MRSA in different countries are as follow: – In Hong-Kong, 6.8% of 455 chicken meat, from Quebec, Canada, and to characterize LA-MRSA isolates total of 309 retail chicken, MRSA was found in 4 samples out of the 309 retail chicken meat samples for an estimated prevalence of 1.3% (Table 2) [51].
Table 2: Prevalence of Staphylococcus aureus from meat in the Africa
|
Countries |
Prevalence |
Reference |
| Algeria | 29.4% | Chaalal et al., 2018 |
| Ethiopia | 34.3% | Hassan et al., 2018 |
| Morocco | 40.38% | Ed-Dra et al., 2018 |
| Ghana | 45% | Effah et al., 2018 |
| Egypt | 15% | Osman et al., 2015 |
Prevalence of Staphylococcus aureus from Meat in the Africa
The contamination of meat by S. aureus across the food chain is a complicated process. The contamination may originate from animals, as well as from humans. Improper hygiene at that level should be avoided to reduce the odds of meat contamination and food poisoning. The main factors that influence the level of contamination are the length at which animals are transported and the methods which are used to move animals from one place to another, holding conditions, geographic location, as well as climate changes (Table 3).
Table 3: Prevalence of Staphylococcus aureus from meat in the Ethiopia
|
City |
Prevalence |
Reference |
| Bahirdar | 54.45% | Bizuneh et al., 2020 |
| Addis Ababa | 29.17% | Kibrom, 2017 |
| Jigjig | 32.22% | Ayalew et al., 2015 |
| Mekelle | 40% | Gurmu et al., 2013 |
| Debre-Zeit | 36.5% | Senait and Moorty, 2016 |
Prevalence of Staphylococcus aureus from Meat in the Ethiopia
In the above table there is difference between prevalence in the different years and cities, this may be due to the degree of meat contamination at food handling, level of environmental hygiene and the degree of awareness related to microbial contamination. The highest incidence of disease usually occurs in people with poor personal hygiene, people subject to overcrowding and children. The European Union estimated that the additional costs of MRSA infections are €380 million annually. In United States different research reported that increase in costs for treating a patient with a MRSA infection compared to a methicillin susceptible Staphylococcus aureus (MSSA) infection range from $3836 – $13,901 per patient per incident. Mortality rates for MRSA and MSSA disease are also increased [52].
Antimicrobial Resistance in Staphylococcus aureus from Meat
Staphylococcus aureus can develops antimicrobial resistance through mutation and horizontal transfer of resistance genes. The most mechanisms which are used to resist the action of antimicrobials include, the production of enzymes that inactivate or destroy the antimicrobial; a reduction of the bacterial cell wall permeability limiting the antimicrobial access into the cell; the development of alternative metabolic pathways to those inhibited by the antimicrobial; and active elimination of the antimicrobial from the bacterial cell or the target site. The new mec gene called which called mecD can confers resistance to all β-lactams antimicrobials, including anti-MRSA cephalosporins, ceftobiprole, and ceftaroline. The mecD gene was in an island of resistance associated with a site-specific integrase, which implies a risk of transmission by horizontal gene transfer to other species [53].
Mechanism of Antimicrobial Drug Resistance
Penicillin Resistance
Penicillin G was discovered in 1928 by Alexander Fleming and the drug was used in human as chemotherapeutic agent in 1941. This antimicrobial was the most common used to treat fatal Gram positive pathogens including Staphylococcal infections. Penicillin resistance of S. aureus is highly prevalent with up to 86% of clinical S. aureus isolates being resistant to the antibiotic in the US. Similar finding was made in Australia and recorded 80% of S. aureus isolates were resistant to penicillin. Staphylococci can produce penicillin resistance by inducing enzyme penicillinase or beta-lactamase encoded by the blaZ gene. This enzyme have ability breakdown the beta-lactam ring of penicillin which lead to inactivation of the antibiotic [54].
Methicillin Resistance
Methicillin Resistance which is also called penicillin’s-stable in S. aureus is characterized as resistance to all β-lactam antibiotics. Because of the presence of resistance gene (mecA) that can stops β-lactam antibiotics from inactivating enzymes. The mecA is a biomarker gene that is responsible for resistance to methicillin and other β-lactam antibiotics by expression of foreign antigens (PBP and PBP2a) that can bind to penicillin. The PBP and PBP2a are resistant to the action of methicillin. Synthesis of PBP2a is controlled and kept at low level, but the level of synthesis can be enhanced if mutations occur in the regulatory genes (https://en.wikipedia.org, 2021b). Additionally, MRSA has a mobile genetic element which called staphylococcal cassette chromosome (SCCmec). The SCCmec carries the mecA gene to encode altered PBP (PBP2a) these binding proteins decrease the ability of β-lactam antibiotics and the MRSA strains can survive in the presence of β-lactam antibiotics [55,56].
Vancomycin Resistance
Vancomycin-resistant S. aureus is a strain of S. aureus that has become resistant to the glycopeptides. This drug was primary observed from a microbial source which is called Streptomyces Orientalis in 1952 and approved for use in 1958. This drug is the first line drug of choice for MRSA infections. The first, reduced vancomycin susceptibility in S. aureus was reported in 1997 in Japan. This resistance mechanism can be occurred by inhibiting the transpeptidation of the peptidoglycan layer in the bacterial cell wall by binding to the C-terminal D-ala-D-ala of the peptidoglycan stem pentapeptide, which prevents the interaction between the penicillin binding proteins and their substrate [57]. The binding between Vancomycin and bacterial cell wall with D-alanyl-D-alanine can inhibits the elongation and cross-linking of bacterial cell wall peptidoglycans, although repressing cell wall synthesis and proceeds to bacterial death. Today, different researchers can divide vancomycin-resistant Staphylococcus aureus into three types: Vancomycin-resistant Staphylococcus aureus, vancomycin-intermediate Staphylococcus aureus and heterologous vancomycin resistant Staphylococcus aureus [58].
Macrolide Resistance
The mechanism of antibiotic resistance development in S. aureus to macrolide, lincosamides can happen when there is the occurrence of methylation at the receptor binding site on the ribosomes. However, this methylation can be catalyzed by a methylases enzyme that is encoded by ribosome methylationmthrough erythromycin methylases enzymes erm and mediated by an efux pump system encoded by mrsA.
Quinolone Resistance
Predominantly the mechanism of action of quinolones was act on DNA gyrase, which is an enzyme that relieves DNA supercoiling and topoisomerase. These antimicrobials can develop resistance due to marked by a gradual acquisition of chromosomal mutations. This action can take place at gyrase and ParC (GrlA in S. aureus) of topoisomerase [59].
Diagnosis and Treatment of S. aureus
The diagnosis of S. aureus pathogen was based on laboratory examination techniques, isolation and identification method. Among the bacteriological examination techniques, the common used for isolation and identification of this pathogen are includes: – Serological and biochemical tests such as catalase, DNase and coagulase tests are used to identify the strain of S. aureus. The most common samples or specimens collected for laboratory examination for this pathogen include: – Blood, sputum, tracheal aspirate, pus, and surface swab. During examined under microscope after employing Gram staining techniques, the organism presence with Gram-positive grape-like cocci in clusters, or pairs. Biochemical test is also the techniques that uses for isolation and identification of this pathogen. Mannitol salt agar is a selective medium that used to isolate S. aureus and S. aureus produces different types of haemolysis including beta-haemolysis, alpha haemolysis and gamma haemolysis on blood agar media (https://microbiologyclass.com/).
The treatment of the Staphylococcus aureus was based on the strain of the infection whether it is resistant to methicillin antibiotic (MRSA) or sensitive to methicillin antibiotics (MSSA). S. aureus infections must be treated with antibiotics, especially in elderly, young, and immune-compromised patients. Skin infections can be treated topically with antibiotic creams. Antibiotic that used for treatment of MRSA includes vancomycin, clindamycin and a combination of antimicrobials that are resistant for bacterial strains. Penicillin is used for non-resistant S. aureus infections (https://biologydictionary.net, 2020). Before treating the affected person as well as humans the physicians must be doing the antibiotic sensitivity test. The most common used antibiotics against this bacteria/pathogen are penicillin, tetracycline, streptomycin, novobiocin, sulfonamides, lincomycin, and spectinomycin. But currently most bacteria are resistant to penicillin and other variety of antibiotics. However, at this time Vancomycin most effective drug of choice against this pathogen.
Anti-virulence or anti–toxin compound is the best option used to treat S. aureus strain pathogen, especially those produce toxin because of this compound does not affect bacterial viability or growth. This anti virulence compound can inhibit bacterial virulence genes, and leads decreasing the ability of pathogen to colonize the host and inversely allow the host innate immunity/biomarkers to eradicate the attenuated pathogen [60]. According to the report from Cordeiro et al. Lysostaphin drug was the most effective than mupirocin in rat models, but there is no any trials are applied for human. Additionally, both thymol and carvacrol are the phenolic terpenoids that are effective antimicrobial activity against S. aureus [61]. Again Daptomycin, a cyclic lipopeptide molecule, is a novel antibiotic that used for vancomycin-unresponsive S. aureus disease. This drug can damages the cytoplasmic membrane of bacteria and leads the protein synthesization [62]. The pathogenic S. aureus is resistant to different antibiotics that previously used to treat this pathogen like; cephalosporins, vancomycin, methicillin, oxacillin and penicillins. Drainage of the fluids or pus in abscess caused by S. aureus can be employed in the management of pus-infections mediated by the pathogen. Treating food poisoning Staphylococcus aureus by fluid and electrolyte were used to boost the immune system of the patient (https://microbiologyclass.com).
Mupirocin is also another antibiotic that used to treat impetigo and nasal decolonization infection of S. aureus. Mupirocin can inhibit the protein synthesis. Fusidic acid is an antibiotic that binds to bacterial elongation factor G and leads to impaired translocation process and inhibition of protein synthesis. This antibiotic has potent activity against S. aureus and clinically used in treatment of mild to moderately severe skin and soft-tissue infections, for example, impetigo, folicullitis, erythrasma, furunculosis, abscesses and infected traumatic wounds. For treating S. aureus strain that develops the biofilm formation, not only antibiotic treatment is effective, in addition to antibiotics using alternative treatment like postsurgical antibiotics was effective. Novel treatments for S. aureus biofilm involving nano silver particles, bacteriophages, and plant derived antibiotic agents effects against S. aureus embedded in biofilms (https://en.wikipedia.org).
Prevention and Control
The control and prevention methods of staphylococcus aureus disease was based on the practice of proper hygienic and individual protection at abattoir and hospital areas. Currently, there is no vaccine available to prevent staphylococcal diseases or infections, due to this reason individuals and hospital institutions must be implement the individual and environmental hygienic practices like hand washing and proper disinfection. Teaching the societies regarding to the protection method of the pathogen such as contaminated foods should be avoided; and food handlers should always observe proper hygiene in the handling, processing, preparation and distribution of food in order to avoid the outbreak of food poisoning due to Staphylococcus aureus (https://microbiologyclass.com). Educate hospital staff based on how hand hygiene can be important in order to protect this bacterium. Narrow-spectrum antibiotics, is used to control decolonization in patients planned for high-risk surgical procedures. Affected group might be recommended antibiotics to eliminate the bacteria, like mupirocin (www.health.vic.gov.au).
Public Health Importance
S. aureus is a major pathogen of public health concern throughout the world, this is due the pathogen can produce Staphylococcal food poisoning. Meat and meat products of animal origin are one of the main sources of staphylococcal food poisoning. Symptoms of Staphylococcus poisoning which include diarrhea, abdominal cramps, vomiting, and nausea occur after consuming toxin-contaminated food. The emergence of antimicrobial resistance, especially the multidrug resistance strain of S. aureus becomes an emerging zoonotic issue for worldwide. Because the resistant organisms fail to respond to first-line treatment, hence, leading to high cost of treatment, prolonged illness and high risk of death with its concomitant financial burden and loss in man-hour to families and societies [63]. Multi Drug resistant staphylococci can affect the health care system by causing prolonged hospitalization, increases the costs of treatments and patient mortality.
Zoonotic bacteria or pathogen can transmit to human through direct contact with animals or indirectly through the food of animal origin. The most common population at risk with zoonotic pathogen are farmers, veterinarians, farm laborers and abattoir workers is greater risk of being colonized or even infected with zoonotic pathogen. Humans may represent an important source of new bacterial strains, which can cause disease in livestock and, as such, pose a potential threat to food security. According to the recent research, the epidemic S. aureus clones in human and animal hosts, Both LA-MRSA ST398 and S. aureus ST5 clone, can causes lameness in poultry, have been shown to originate from humans but have now adapted and diversified to spread in animal hosts [64]. According to different researcher the organisms can be transferred to animals, and re-transmitted from this source to humans (reverse transmission) [65]. Different researcher reports the presence of Methicillin-resistant S. aureus in chicken meats, because of contamination and is considered a source of human infections caused by consuming contaminated meat of animal origin [66] Administering of under dose drugs to food animals can leads the pathogen to carry antimicrobial resistance genes or plasmids, which makes the multiplication and transmission of those genes among strains. This means using low dosage of antibiotics can initiates the transmission of resistance between different hosts including humans, animals and the environment [67]. The incidence rate of S. aureus disease was highest among the people with poor personal hygiene, overcrowding and children. But, staphylococcal disease may affect all people and animals. Healthcare employees, football players, prison inmates, people in day-care centers, people in military quarters, homeless people, intravenous drug users and men who have sex with men are also among the most people at risk (www.health.vic.gov.au).
Economic Impact of S. aureus
In Europe, Asia and North America, there is an increasing level of MRSA due to epidemics of highly transmissible. Due to the increasing incidence rate of MSSA and MRSA diseases and it increase in load of bacteremia and costs for treatment. This will causes economic problems, especially for developing countries there is scarcity of effective drugs and failure of treatment due to inappropriate antimicrobials or lack of efficacy of anti-MRSA drugs, excess toxicity of will causes to increase the morbidity and mortality. Drug-resistant infections also affect patients’ social and economic status by increasing healthcare costs, mortality and morbidity, and decreasing productivity. Among countries where use has been successfully reduced, significant investments were necessary to improve biosafety and biosecurity on farms in order to enable intensive production systems without the use of antimicrobials. Similar measures could be implemented in newer facilities in LMICs but may be too expensive for small livestock operations that lack the necessary technical and financial resources. Regardless, the benefits of reducing national resistance rates are predicted to outweigh the costs of introducing such bans. One study predicted that a worldwide ban on antimicrobial growth promoters would lead to a decrease of 1% to 3% in global meat production and a loss in meat production value of US$ 13.5 to US$ 44.1 billion, compared to an estimated loss of US$ 35 billion per year in the United States alone due to healthcare costs and losses to productivity from AMR [68-85].
Conclusion and Recommendation
Staphylococcus aureus is a Gram-positive, facultative anaerobic bacterium which grows individually, in pairs, short chains or grape-like clusters. The bacterium is catalase and coagulase positive, oxidase-negative, non-motile microorganism that does not form spores. Staphylococcus aureus can causes different diseases such as abscess in deep organs, toxin mediated diseases, self-limiting skin infections to life-threatening pneumonia, osteomyelitis, endocarditis, septicemia, Foodborne-illness and toxic shock syndrome (TSS). Foods contaminated with S. aureus are a potential vehicle for the transmission of enterotoxigenic S. aureus to humans. Staphylococcus aureus is a foodborne pathogen which is responsible for contamination of different food products and results food spoilage, reduction of food safety and shelf life and cause foodborne poisoning via production of deadly enterotoxins. S. aureus is a very versatile human pathogen that readily adapts to changing environments and acquires antibiotic resistance genes through a number of different mechanisms. Antimicrobial resistance is a serious threat to public health across the globe. A wide variety of antimicrobial drugs are employed to treat S. aureus infections. However, emergence and spread of antimicrobial resistant S. aureus isolates constitute a global challenge for the effective treatment and control of these infections.
Therefore, based on the above conclusion, the following recommendations are forwarded:-In the future the researcher:
- Should focus on developing a safe vaccine that contains secreted as well as cell wall-associated antigens that evoke a sustained protective response over a significant period of time.
- Should utilize information on the variation, distribution and function of surface protein antigens amongst aureus lineages to ensure that cocktails of gene variants are included in the vaccine.
- Should focus on the unraveling of the cellular immune responses directed against aureus.
- proper handling of raw meat, adequate cleaning of hands, surfaces, equipment’s, disinfection of slaughter houses, vehicles and good personal hygiene can reduce spreading of Staphylococcus through meat.
- The occurrence of multidrug resistance Staphylococcus particularly aureus should be under consideration during selection of antimicrobials for the treatment.
- Multiple drug resistant Staphylococcus aureus have a wide distribution in different meat of animal origin and therefore care should be taken in to account during processing to destroy the micro-organisms to avoid the risk of human infection.
Acknowledgment
I would like to start by extending gratitude and praise to Almighty Allah, the kindest and most merciful, for keeping us well and bestowing upon us the unwavering resolve, bravery, strength, and endurance needed to complete this difficult endeavor. The person who controls the course of advancement is Dr. Daniel Shiferaw (DVM, MSC, Assist Prof), who is my advisor. Words can’t quite explain how grateful I am for his constant constructive criticism, diligent scientific advice, and untold hours spent editing this work. Last but not least, we would want to express how grateful we are to Haramaya University Faculty of Veterinary Medicine for providing the necessary facilities.
Abbreviations
Agr: Accessory Regulatory Gene; AMR: Antimicrobial Resistant; CA-MRSA: Community-Associated Multi Drug Resistant Staphylococcus aureus; DNA: Deoxy Nucleic Acid; HA-MRSA: Hospital-Associated Multi Drug Resistant Staphylococcus aureus; HIV: Human Immunodeficiency Virus; LA-MRSA: Livestock-Associated Multi Drug Resistant Staphylococcus aureus; MRSA: Multi Drug Resistant Staphylococcus aureus; PBP: Penicillin-Binding Protein; PSM: Phenol Soluble Moduli’s; SCCmec: Staphylococcal Cassette Chromosome mec; SCV: Small Colony Variant; TSS: Toxic Shock Syndrome; σB: Sigma Factor.
References
- Rasoul Y, Mashouf Seyed M, Hosseini Seyed M, Mousavi and Mohammad R, Arabestani (2014) Prevalence of Enterotoxin Genes and Antibacterial Susceptibility Pattern of Staphylococcus aureus Strains Isolated from Animal Originated Foods in West of Iran. Oman Medical Journal 30: 283. [crossref]
- Ronaq Zaman, Muhammad Inam, Zobia AF (2013) Sensitivity Pattern of Staphylococcus Aureus Isolates to Commonly Used Antibiotics. Pakistan Journal of Medicine and Health Science 7(3):651.
- U. Olugbue, V. O. Nwaugo, M. C. Korie, M. O. Okata, I. Oko and N. U. O (2018) Antimicrobial Susceptibility Profiles of Staphylococcus aureus Strains from Ear, Nose and Wound Swabs of Patients Attending Health Care Facilities, Ebonyi Sate, Nigeria. Microbiology Research Journal International. 3973123:1: 1.
- Frederick Adzitey, Rejoice Ekli and Martin Aduah. 2020. Incidence and antibiotic susceptibility of Staphylococcus aureus isolated from ready to eat meats in the environs of Bolgatanga Municipality of Ghana. Cogent Environmental Science 6: 1791463:
- Lika, E.; Puvaˇca, N.; Jeremi´c, D.; Stanojevi´c, S.; Shtylla Kika, T.; Cocoli, S.; de Llanos Frutos, R (2021) Antibiotic Susceptibility of Staphylococcus Species Isolated in Raw Chicken Meat from Retail Stores. Antibiotics 10: 904: 1-2. [crossref]
- Piyali Das, Pranab Behari M (2016) Prevalence of Staphylococcus in raw meat samples in Southern Assam, India. IOSR Journal of Agriculture and Veterinary Science 9(1):23.
- Bizuneh Tsehayneh, Taddesse Yayeh, Birhan Agmas and Semahegn Y (2021) Valuation of Bacterial Load and Antibiotic Resistance Pattern of Staphylococcus aureus from Ready-to-Eat Raw Beef in Bahir Dar City. International Journal of Microbiology 10(1155-5560596): 2-6. [crossref]
- Nwankwo Emmanuel Onwubiko andb Nasiru Magaji Sadiq.(2018) Antibiotic sensitivity pattern of Staphylococcus aureus from clinical isolates in a tertiary health institution in Kano, Northwestern Nigeria. The Pan African Medical Journal 8(4):2.
- Narin A Rasheed and Nawfal R H. 2021. Staphylococcus aureus: An Overview of
Discovery, Characteristics, Epidemiology,Virulence Factors and Antimicrobial Sensitivity. European Journal of Molecular & Clinical Medicine 8(3): 1161-1169. - Jhalka Kadariya, Tara C. Smith, and Dipendra Thapaliy (2014) Staphylococcus aureus and Staphylococcal Food-Borne Disease: An Ongoing Challenge in Public Health. Hindawi Publishing Corporation Biomedical Research International 827965: 6.
- Lesley Maurice Bilung, Ahmad Syatir Tahar, Rosdi Kira, Aina Ariffah Mohd Rozali,
and Kasing Apun (2018) High Occurrence of Staphylococcus aureus Isolated from Fitness Equipment from Selected Gymnasiums. Hindawi Journal of Environmental and Public Health 2018: 4592830: 1. [crossref] - Alexandra Fetsch and Sophia Johler (2018) Staphylococcus aureus as a Foodborne Pathogen. Current Clinical Microbiology Reports.
- Arumugam Gnanamani, Periasamy Hariharan and Maneesh Paul-Satyaseela (2017) Staphylococcus aureus: Overview of Bacteriology, Clinical Diseases, Epidemiology, Antibiotic Resistance and Therapeutic Approach.Staphylo coccus Aureus: Intech Open Access books 54154: 4-12.
- Biology dictionary.net Editors. Staphylococcus Aureus. Biology Dictionary 14 May 2020.Accessed on November 22, 2021.
- Tracey A. Taylor; Chandrasekhar G. Unakal (2021) Staphylococcus Aureus. NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health 441868 (28722898): 2-3. [crossref]
- Christina J. Heaton, Gracen R. Gerbig, Lucas D. Sensius, Vishwash Patel and Tara C. Smith (2020) Staphylococcus aureus Epidemiology in Wildlife: A Systematic Review. Antibiotics 9: 1-2. [crossref]
- Uka, K.K, Oguoma, S.I, Chukwu, C.A. and Emele, C.I (2020) Adoption of Artificial Intelligence for Diagnosis and Treatment of Staphylococcus aureus Infections Disease on Humans. E-Health Telecommunication Systems and Networks 9: 1-4.
- Henok Ayalew Tegegne, Amare Berhanu, Yitbarek Getachew, Biresaw Serda, Dagmar Nölkes, Sissay Tilahun, Berhanu Sibhat (2019) Microbiological safety and hygienic quality of camel meat at abattoir and retail houses in Jigjiga city, The Journal of Infection in Developing countries 13;3: 189. [crossref]
- Matewos Kebede Kassa (2020) The Prevalence, Distribution of Staphylococcus and its Antimicrobial Susceptibility Status of the Isolates from Meat and Dairy Milks of Bishoftu, Ethiopia. International Journal of Advanced Research in Biological Sciences 7;3: 153.
- Matewos Kebede Kassa (2020) The Prevalence, Distribution of Staphylococcus and its Antimicrobial Susceptibility Status of the Isolates from Meat and Dairy Milks of Bishoftu, Ethiopia. International Journal of Advanced Research in Biological Sciences 7: 3: 153.
- Smith TC (2015) Livestock-Associated Staphylococcus aureus: The United States Experience. PLOS Pathogens 11(2):4.
- Andarge Zelalem, Mekonnen Sisay, Jessie L. Vipham, Kebede Abegaz, Ameha Kebede and Yitagele Terefe (2019) The prevalence and antimicrobial resistance profiles of bacterial isolates from meat and meat products in Ethiopia: a systematic review and meta-analysis. International Journal of Food Contamination 6(1): 2.
- Onuoha, S.C, Ani, T. P, Oko, F.N, Ovia, K.N (2020) Prevalence of antibiotic resistant staphylococcus aureus in raw meat samples intended for human consumption. International Journal of Biology, Pharmacy and Allied science 9(3): 345-346.
- Abunna F, Abriham T, Gizaw F, Beyene T, Feyisa A. 2016. Staphylococcus: Isolation, Identifcation and Antimicrobial Resistance in Dairy Cattle Farms, Municipal Abattoir and Personnel in and Around Asella, Ethiopia. Journal of Veterinary Science and Technology 7(6): 2.
- Shawish RR, Al-Humam NA (2016) Contamination of beef products with staphylococcal classical enterotoxins in Egypt and Saudi Arabia. GMS Hygiene and Infection Control 11(8):5. [crossref]
- Amjad Islam Aqib, Muhammad Ijaz, Muhammad Shoaib, Iqra Muzammil, Hafiz Iftikhar Hussain, Tean Zaheer, Rais Ahmed, Iqra Sarwar, Yasir Razzaq Khan and Muhammad Aamir Naseer, (2021) Staphylococcus aureus and Dairy Udder, Insights into Drug Resistance in Staphylococcus aureus, Amjad Aqib, IntechOpen.
- Crespo‑Piazuelo and Lawlor (2021) Livestock‑associated methicillin‑resistant Staphylococcus aureus (LA‑MRSA) prevalence in humans in close contact with animals and measures to reduce on farm colonization. Irish Veterinary Journal 74(21): 2-3. [crossref]
- Haag AF, Fitzgerald JR, Penadés JR (2019) Staphylococcus aureus in animals. Microbiol Spectrum 7(3): 5-6.
- Mulemba Tillika Samutela, Geoffrey Kwenda, Edgar Simulundu, Panji Nkhoma,
Hideaki Higashi, Andrew Frey, Matthew Bates, Bernard M. H (2021) Pigs as a potential source of emerging livestock-associated Staphylococcus aureus in Africa: a systematic review. International Journal of Infectious Diseases 109:39. [crossref] - Christina J. Heaton, Gracen R. Gerbig, Lucas D. Sensius, Vishwash Patel and Tara C. Smith (2020) Staphylococcus aureus Epidemiology in Wildlife: A Systematic Review. Antibiotics 9:89: 1-2. [crossref]
- Muhammad Farhab, Muhammad Tahir Aleem, Shakseema Shaukat, Ayesha Qadry, Muhammad Zeeshan Ul Haq, Fateh Ullah, Muhammad Jawad and Amjad Islam Aqib (2021) Staphylococcus aureus and the Veterinary Medicine, Insights into Drug Resistance in Staphylococcus aureus. Intech open.
- Maliha Gulza and Asima Zehra (2018) Staphylococcus aureus: A brief review. International Journal of Veterinary Science and Research.
- Peng Gaoa, Pak Leung Hoab, Bingpeng Yana, Kong Hung Szea, Julian Daviesc and Richard Yi Tsun K (2018) Suppression of Staphylococcus aureus virulence by a small molecule compound. PNAS 115(31): [crossref]
- Foster TJ, Geoghegan JA, Ganesh VK, Höök M (2014) Adhesion, invasion and evasion: The many functions of the surface proteins of Staphylococcus aureus. Nature Reviews Microbiology 12(1): 1-2. [crossref]
- Kavitha Shettigar and Thokur Sreepathy Mura (2020) Virulence factors and clonal diversity of Staphylococcus aureus in colonization and wound infection with emphasis on diabetic foot infection. European Journal of Clinical Microbiology and Infectious Diseases 39:2237. [crossref]
- Valeria Velasco, Mario Quezada-Aguiluz and Helia Bello-Toledo (2019) Staphylococcus aureus in the Meat Supply Chain: Detection Methods, Antimicrobial.
- Gordon Y. C. Cheung, Justin S.B and Michael (2021) Pathogenicity and virulence of Staphylococcus aureus. Virulence 12(1):556.
- Jelle Vlaeminck, Dina Raafat, Kristin Surmann, Leen Timbermont, Nicole Normann, Bret Sellman, Willem J. B. van Wamel and Surbhi Malhotra K (2020) Exploring Virulence Factors and Alternative Therapies against Staphylococcus aureus Toxins 12:721: 5. [crossref]
- Roberto Adame-Go´mez, Natividad Castro-Alarco´n, Amalia Vences-Vela´zquez,
Jeiry Toribio-Jime´nez, Abigail Pe´rez-Valdespino, Marco- Antonio Leyva-Va´zquez, and Arturo Ram´ ırez-Peralta (2020) Genetic Diversity and Virulence Factors of aureus Isolated from Food, Humans, and Animals. Hindawi International Journal of Microbiology (2020)(1048097): 2. - Yilmaz, E.S. and Aslantas, O (2017) Antimicrobial resistance and underlying mechanisms in Staphylococcus aureus Asian Pacific Journal of Tropical Medicine 10(11): 1059-1064. [crossref]
- Nadira Mourabit, Abdelhay Arakrak, Mohammed Bakkali, Zeineb Zian, Joaira Bakkach, and Amin Laglaoui (2021) Antimicrobial Resistance Trends.
- Zhou Kaixiang Chao Li Dongmei Chen Yuanhu Pan Yanfei Tao wei Qu Zhenli Liu Xiaofang wang Shuyu Xie (2018) A review on nanosystems as an effective approach against infections of Staphylococcus aureus. International Journal of Nano medicine 13:7335. [crossref]
- Alejandro De Jesús Cortés-Sánchez, Mayra Díaz-Ramírez, Ma. De la Paz Salgado-Cruz and Rocío G. HernandezNava (2020) Food Safety and Fish Production the Case of Staphylococcus aureus: A Review. Online Journal of Biological Sciences 20 4: 294-299.
- Liyun Shi, Huanhuan Wang and Zhe Lu. 2016. Staphylococcal Infection and Infertility, Genital Infections and Infertility. IntechOpen.
- Thwala, T.; Madoroba, E.; Basson, A.; Butaye, P (2021) Prevalence and Characteristics of Staphylococcus aureus Associated with Meat and Meat Products in African Countrie. Antibiotics 10:1108: 1-4. [crossref]
- Piva S, Mariella J, Cricca M, Federica Giacometti, Angelo Romano and Andrea Serraino (2021) Epidemiologic case investigation on the zoonotic transmission of Staphylococcus aureus infection from goat to veterinarians. Zoonoses Public Health 68:685. [crossref]
- Park S, Ronholm J (2021) Staphylococcus aureus in agriculture: lessons in evolution from a multispecies pathogen. Clinical Microbiology Reviews 34(2): 11-16. [crossref]
- Qekwana, Daniel Nenene; Oguttu, James Wabwire; and Odoi, Agricola (2019) “Geographic distribution of Staphylococcus spp. infections and antimicrobial resistance among dogs from Gauteng Province presented at a veterinary teaching hospital in South Africa. Faculty Publications and Other Works Biomedical and Diagnostic Sciences (https://trace.tennessee.edu/utk_compmedpubs/117) Accessed on December 12, 2021.
- Birhan Agmas ,Bizuneh Tsehayneh and Taddesse Yayeh (2020) Staphylococcus Aureus Health Risk from Ready-To-Eat Raw Beef Meat and Associated Risk Factors in North West Ethiopia. Scholarly Journal of Food and Nutrition 3(2): 348-350.
- Wardhana DK, Haskito AEP, Purnama MTE, Safitri DA, Annisa S (2021) Detection of microbial contamination in chicken meat from local markets in Surabaya, East Java, Indonesia. Veterinary World 14(12): 3138. [crossref]
- Bernier-Lachance J, Arsenault J, Usongo V, Parent E´, Labrie J, Jacques M, et al. (2020) Prevalence and characteristics of LivestockAssociated Methicillin-Resistant Staphylococcus aureus (LA-MRSA) isolated from chicken meat in the province of Quebec, Canada. PLoS ONE 15(1): 1-2. [crossref]
- Wanda Reygaert (2014) Antimicrobial resistance mechanisms of Staphylococcus aureus. Research Gate. C. Reygaert Department of Biomedical Sciences, Oakland University William Beaumont School of Medicine, Rochester, MI, USA (https://www.researchgate.net/publication/267695121). [crossref]
- Schwendener S, Cotting K, Perreten V (2017) Novel methicillin resistance gene mecD in clinical Macrococcus caseolyticus strains from bovine and canine sources. Scientific Reports 7:43797:2. [crossref]
- Jactty Chew, Suat-Cheng Peh and Teow Sin Yeang (2018) Non-microbial Natural Products That Inhibit Drug Resistant Staphylococcus aureus Chp1. Intechopen 10: 5772-74588.
- Zhu Li (2018) A Review of Staphylococcus aureus and the Emergence of Drug-Resistant Problem. Advances in Microbiology 8: 2165-3410.
- Anderson Clayton da Silva, Marjory Xavier Rodrigues and Nathália Cristina Cirone Silva (2019) Methicillin-resistant Staphylococcus aureus in food and the prevalence in Brazil: a review. Brazilian Journal of Microbiology 51:349. [crossref]
- Bitrus, A.A, O.M. Peter, M.A. Abbas and M.D. Goni (2018) Staphylococcus aureus: A Review of Antimicrobial Resistance Mechanisms. Journal of Veterinary Sciences: Research and Reviews 4(2): 47-58.
- Guo Y, Song G, Sun M, Wang J and Wang Y (2020) Prevalence and Therapies of Antibiotic-Resistance in Staphylococcus aureus. Frontiers in Cellular and Infection Microbiology 10:107.
- Irina Gheorghe, Marcela Popa and Luminiţa Gabriela M (2018) Molecular Features of Virulence and Resistance Mechanisms in Nosocomial and Community-Acquired Staphylococcus aureus. Intech Open.
- Daniela Bencardino, Giulia Amagliani, Giorgio Brandi (2021) Carriage of Staphylococcus aureus among food handlers: An ongoing challenge in public health. Food Control 130:108362: 7-8.
- Kong, C.; Neoh, H.M.; Nathan, S (2016) Targeting Staphylococcus aureus toxins: A potential form of anti-virulence therapy. Toxins 8:72:6.
- Mohini Bhattacharya, Daniel J Wozniak, Paul Stoodley, and Luanne HallStoodley (2016) Prevention and treatment of Staphylococcus aureus biofilms. Expert Review Anti Infection Therapeutics 13(12): 6.
- Mahendra Pal, Gemechu Berhanu Kerorsa, Lencho Megersa Marami, and Venkatara Kandi (2020) “Epidemiology, Pathogenicity, Animal Infections, Antibiotic Resistance, Public Health Significance, and Economic Impact of Staphylococcus Aureus: A Comprehensive Review.” American Journal of Public Health Research 8(1):15-19.
- Tracy Schmidt, Marleen M. Kock and Marthie M. Ehlers (2015) Antimicrobial Resistance in Staphylococci at the Human-Animal Interface IntechOpen 103-104.
- Spickler, Anna Rovid (2016) Methicillin Resistant Staphylococcus aureus (http://www.cfsph.iastate.edu/DiseaseInfo/factsheets).
- B. Kim, K. W. Seo, H. Y. Jeon, S.-K. Lim and Y. J. Le (2018) Characteristics of the antimicrobial resistance of Staphylococcus aureus isolated from chicken meat produced by different integrated broiler operations in Korea. Poultry Science Association Inc 97: 962.
- Verónica Karen Castro Péreza, Geraldo Márcio da Costaa, Alessandro Sá Guimarãesb, Marcos Bryan Heinemannc, Andrey Pereira Laged, Elaine Maria Seles Dorneles (2020) Relationship between virulence factors and antimicrobial resistance in Staphylococcus aureus from bovine mastitis. Journal of Global Antimicrobial Resistance 22: 793. [crossref]
- Laxminarayan R, Van Boeckel TP, Teillant A (2015) The Economic Costs Of Withdrawing Antimicrobial Growth Promoters From The Livestock Sector. OECD Food, Agriculture and Fisheries Papers 78: 33.
- Abunna F, Abriham T, Gizaw F, Beyene T, Feyisa A (2016) Staphylococcus: Isolation, Identifcation and Antimicrobial Resistance in Dairy Cattle Farms, Municipal Abattoir and Personnel in and Around Asella, Ethiopia. Journal of Veterinary Science and Technology 7(6): 2.
- Chaalal W, Chaalal N, Bouraf N, Kihal M, Diene SM and Rolain JM (2018) Characterization of Staphylococcus aureus isolated from food products in Western Algeria. Foodborne Pathogen Disease 15(6): 353. [crossref]
- Dehkordi FS, Gandomi H, Basti, AA, Misaghi A and Rahimi E (2017) Phenotypic and genotypic characterization of antibiotic resistance of methicillin-resistant Staphylococcus aureus isolated from hospital food. Antimicrob Resistant Infection Control 6 (1): 104. [crossref]
- Ed-Dra A, Filali, FR, Bouymajane A, Benhallam F, El Allaoui A, Chaiba, A and Giarratana, F (2018) Antibiotic susceptibility profile of Staphylococcus aureus isolated from sausages in Meknes, Morocco. Veterinary World 11(10): 1459.
- Endalle Gurmu and H. Gebretinsae (2013) Assessment of bacteriological quality of meat cutting surfaces in selected butcher shops of Mekelle city, Ethiopia,” Journal of Environmental and Occupational Science 2(2):61.
- Gutiérrez D, Fernández L, Martínez B, Ruas-Madiedo P, García P and Rodríguez A (2017) Real-Time Assessment of Staphylococcus aureus Biofilm Disruption by PhageDerived Proteins. Microbiology 8: 1632.
- Ayalew, A. Berhanu, B. Sibhat, and B. Serda, (2015) Microbiological assessment of meat contact surfaces at abattoir and retail houses in Jigjiga town, Somali National Regional State of Ethiopia,” ISABB Journal of Food and Agricultural Sciences 5(3): 21.
- Vic (Victoria Department of Health) (2015) Stapylococcal infection. Melbourne, Victoria: Department of Health.
- Kavitha Shettigar and Thokur Sreepathy Mura (2020) Virulence factors and clonal diversity of Staphylococcus aureus in colonization and wound infection with emphasis on diabetic foot infection. European Journal of Clinical Microbiology and Infectious Diseases 39:2237. [crossref]
- Margaret Carrel, Michihiko Goto, Marin L, Schweizer, Michael Z David, Daniel Livorsi, and Eli N. Perencevich (2017) Diffusion of clindamycin-resistant and erythromycin resistant methicillinsusceptible Staphylococcus aureus (MSSA), potential ST398, in United States. Veterans Health Administration Hospitals, (2003)-(2014) Antimicrobial Resistance and Infection Control 6: 55. [crossref]
- Microbiology Class (2020) Staphylococcus Aureus. Microbiology Bacteriology 103 (https://microbiologyclass.com).
- Nadira Mourabit, Abdelhay Arakrak, Mohammed Bakkali, Zeineb Zian, Joaira Bakkach, and Amin Laglaoui (2021) Antimicrobial Resistance Trends in Staphylococcus aureus Strains Carried by Poultry in North of Morocco: A Preliminary Analysis. Hindawi, Journal of Food Quality (2021) 8856004: 2.
- Osman KM, Amer AM, Badr JM and Saad AS (2015) Prevalence and antimicrobial resistance profile of Staphylococcus species in chicken and beef raw meat in Egypt journal of Foodborne Pathogen and Disease 12(5): 406. [crossref]
- Senait G and Moorty PA (2016) “Isolation and identification of Staphylococcus species from ready-to-eat meat products in and around Debre-Zeit, Ethiopia,” International Journal of Research 3(4): 6.
- Tracy Schmidt, Marleen M. Kock and Marthie M. Ehlers (2015) Antimicrobial Resistance in Staphylococci at the Human-Animal Interface IntechOpen 103-104.
- D. Karisma, N. Wiqoyah, S. Pusarawati (2021) Prevalence of Escherichia Coli, Salmonella Species, Staphylococcus Aureus Bacteria in Chicken Meat of Traditional Market
Surabaya City. Jurnal Ilmu dan Teknologi Kesehatan 8(2): 195.