DOI: 10.31038/PSC.2022222
Abstract
Systemic Lupus Erythematosus (SLE) is an autoimmune disease characterized by unpredictable multiorgan involvement and a broad range of age of onset and unspecific manifestations. The identification of the onset of the SLE is very complex. The incidence is higher in young women with a peak between 15 and 40 years and a female to male ratio of 6-10:1. In childhood, the incidence is lower by a factor of ten with a female/male ratio=2:1. The variable prevalence is higher in Afro-Caribbean and Asians (207 and 50/100,000 cases, respectively), lower in Caucasians with an incidence of 20/100,000. The disease results from complex and multifactorial interaction of genetic, epigenetic and environmental factors that led to immune dysregulation and loss of tolerance to self antigens. An exaggerated defense response of the body to a noxious stressor as quiescent Epstein Barr Virus infection involves the release of acute-phase reactants, by uncontrolled activation of cytotoxic T lymphocytes, natural killer cells, and macrophages that can lead to a cytokine storm and can cause a massive inflammatory cascade leading to end-organ dysfunction (kidney and liver more frequently) and even death due to a self-mantaining process. We present a case of Septic shock and MOF on childhood untrated SLE.
Keywords
Lupus Eritematosus sistemico, Immunology, Etiopatology, Clinical manifestation, Voluntary avoided therapeutic treatment, Cytosorb, Rescue therapy
Introduction
A 16-year-old female was transferred to our hospital (tertiary care hospital with the only pediatric intensive care of country) on 17 February with a diagnosis of deep respiratory and cardiovascular insufficiency and anuria (Tables 1 and 2).
Table 1: Clinical features of SLE
| Mucocutaneous Manifestations. (face and shoulder) |
| Musculoskeletal Manifestations |
| Hematologic and reticuloendothelial manifestations |
| Neuropsychiatric and Gastrointestinal Manifestations |
| Renal and Liver Manifestations (late onset and life-threatening) |
| Cardiovascular and Pulmonary Manifestations (late onset and life-threatening) |
| Exitus due to MODs. |
Table 2: Epidemiology of SLE
| Male | Age > 40 y | 10.1 on 1000000 |
| Female | 15< age <40 y | 6 on 1000000 |
| Pediatric Ages | Age <16 y | M/F=2:1 |
| Carribean | 207 on 1000000 | |
| Caucasians | 50 on 100000 | |
| Asian | 20 on 100000 |
Past Medical History
Previous diagnosis at 10 years age of “Bullous systemic lupus erythematosus” (BSLE) an uncommon cutaneous presentation that occurs even less frequently in the pediatric population. Unfortunately the patient received inadequate therapeutic treatment with consequent rapid evolution in a severe form of SLE, and in the last two years there wa a rapid worsening of desease expressions in the whole body function leading till the observed rapid evolution in MOF. On admission the patient presented agonic clinical conditions, respiratory failure, bilateral pleural effusion and pulmonary consolidation throughout the area, state of coma (GCS 6-7), hyporesponsiveness to painful stimulation, discrasic oedema of the face and of the lower and upper limbs. A blood gas analysis showed values incompatible with the correct functioning of the metabolic-respiratory systems: PaO2< 50, PCo2 >89; PH 6.86: HCo3-12, BE: -20, Lactacidemia >25.
We proceeded to emergency intubation, mechanical ventilation in PCV and positioning of central vascular accesses to initiate inotropic support in the need to recover the respiratory and metabolic function. Brain protection was performed with morphine, dexdemetomidine and propofol. Fenoldopam infusion, 1 mg/kg/h was started On careful physical examination resulted the presence of muscle-tendon retractions of the major joints due to prolonged immobility and untreated lupus skin lesions. She also presented with an ulcerated bullous lesion, deepened to the tibial bone, suppurating and bleeding in the left lower leg. There were: cold cyanotic skin (rectal temperature 33°C) and the presence of unidentifiable patches spread throughout the body that showed generalized rigidity, a so called “rigor mortis precox”-like state. To study the anasarca state a scan was performed at bedside that found 6,000 ml of ascites,pericardial effusion and bilateral pulmonary consolidations.
Laboratory testing revealed: hypoalbuminemia and significant dysprotidemia, creatininemia> 3 times the basal value, proteinuria>3 gr/dl, persistent anuria from> 12 h (Tables 1-3).
Table 3: Laboratory tests on admission
|
Laboratory tests |
T.I. Ped Admission |
| WBC | 14430 uL |
| Neu | 95.39% |
| Linf | 2.72% |
| RBC | 2.200000 uL |
| HGB | 5.7 gr/dl |
| HCT | 17.48% |
| PLT | 103000 u/L |
| Glicemia | 92 mg/dl |
| Azotemia | 262 mg/dl |
| Creatinina | 3.59 mg/dl |
| Prot. Tot. | 5.8 gr/dl |
| Albumina | 17 gr/L |
| AST | 22 U/L |
| ALT | 11 U/L |
| GGT | 16 U/L |
| LDH | 285 U/L |
| Bil Tot. | 0.27 mg/dl |
| Bil ind. | 0.15 mg/dl |
| Bil dir. | 0.12 mg/dl |
| CPK | 132 U/l |
| Mioglob. | 325 ng/ml |
| PCR | 178 mg/L |
| PCT | 9.44 ng/ml |
| troponina | 17.3 ng/ml |
| PT-INR | 1.16 |
| PTT-Ratio | 1.54 |
| Fibrinog. | 218 mg/dl |
| ATIII | 62% |
| D-dimero | 34072 mg/L |
| Pro-BNP | 72906 pg/ml |
| Presep. | 2748 pg/ml |
CT scan was performed looking for hemorrhagic-ischemic cerebral lesions, with negative result but confirming the massive ascitic effusions in the pelvic cacities and between the viscera as well as in the Epiplon retrocavity, with no other acute organ lesions, except for renal congestion and bilateral alteration of the cortical density of the kidneys. Invasive ventilation and cardiovascular support were modulated. Management included continuous administration of packed Red Blood Cell, repeated administration of Fresh Frozen Plasma, Albumin 19% at 2 ml/h in continuous infusion, heparin infusion 50 IU/Kg/day, provertinum, AT III, Fibrinogen, diuretics and Glucose in adequate percentage (Table 4).
Table 4: Fluids, hematologic therapeutics, cardiovascular support intake after admission
|
Concentrated Blood Red Cells |
250 mls |
250 ml after three/hours |
| Fresh Frozen Plasma | 200 mls plus 200 mls | 200 ml bidaily for 1 week |
| Albumine 19% | %0 ml at 2 ml/hts IV continuos infusio | The same regimen for 10 days |
| Provertinum | 250 mg and 250 mg after 5 hrs | As per needed 150 mg IV |
| AT III | 400 IU and 250 IU after 5 hrs | As per needed on lab test referral |
| Fibrinogen | 259 mg and 250 after 5 hrs | As per needed on lab tests |
| Diuretics | 60 ml bolus followed by 10 mg Hr IV infusion | Untilldismission from ICU |
| Glucose 33% | 10 ml/hr for 6 hrs IV continuous infusion | Only as per parenteral nutrition at 50% of total caloric daily requiring |
| Fenoldopam | 1 mg/kh/day | 1 week (Titrate) |
| Noradrenaline | 0,1 mcg/kg/min | 1 week (Titrate) |
| Adrenaline | 0,1 mcg/kg/min | 8 days (Titrate) |
| Milrinone | 0,5 mcg/kg/min | 25 days (Titrate) |
Blood samples were taken, skin wound swab for PCR’s bacteria detection was negative as weel as throat swab for PCR for viruses and bacteria. Bronchoculture was positive for enterococcus faecium, subsequently, even for Aspergillus Niger treated with Voriconazole. Blood culture and urine culture positive for Candida Albicans treated with Fluconazole. A further examination of the biological parameters showed: leukopenia=2730, lymphopenia and thrombocytopenia 47000 uL, CRP=100 mg/dl, PCT> 1.5 pgr/ml, D-Dimers: 10000 UI/ml, PT INR 2.5 and PTT ratio: 2.7, Fibrinogen=500 mg/dl, LDH> 400 mg/dl, creatinine> 3 mg/l, reduced transaminase values such as chronic liver failure, altered values of ferritin and triglycerides compatible with the initial macrophage-histocytic activation process, albuminemia 12 mg/dl, total protein 2.0 Mg/dl, proteinuria> 3 g/l. Broad-spectrum antibiotic therapy was started and then targeted on antibiogram and culture outcomes, with Teicoplanin, fosfomycin and fluconazole, in rotation during the same hospitalization with Meropemen, Vancomycin, Voriconazole and Sulfamethoxazole trimetropin.
Due to worsening anasarca following the capillary leak and deteriorating renal function Treatment with CVVHD-F was initiated. Under this therapeutic management at the maximum support, in the following hours there wasn’t any improvement, especially persisting the state of severe acidosis mixed with Ph value never above 7.10. In order to control the multiorgan dysfunction caused by septic shock and the state of total functional anergy and dysregulation, presumably triggered by auto cannibalism process, we proposed to the parents the option to aply as rescue therapy the “Cytosorb Adsorber” to try to block the “Cytokine Storm” (that we where convinced was the principal cause of the functional dysfunctions), in an desperate attempt to restore an acceptable energy and metabolic production capable of supporting the life-saving needs of the patient [1-24].
Materials and Methods
Since 2016, in our Unit, a therapeutic project started, initially experimental, later well-defined and applied, for the Adsorber Cytosorb (Cytosorb Corporation-GmBH-Berlin D (E) – (USA) use in immunity dysregulations case in order to stop Cytokine Storm Progression and to initiate a “Rescue Therapy Treatment”, for compassionate purpose in patient in “Imminentia Mortis” condition. In this case, three cycles of CytoSorb Absorber were performed, mounted on Dialysis Machine Prismaflex (Baxter) in a downstream position to the filter used for CVVHD-F. Each cycle lasted 24 hours, circuit anticoagulation was maintained with low molecular weight Enoxaparin at a dose of 15-30 IU/kg/h (while continuing systemic administration of 50 U/I of heparin per day in continuous infusion). The PTT value was maintained at 70 sec and the act (200-220); the dialysis flow was established at 150 ml/min and a blood filtration flow of 200 ml. The priming of the circuit was integrated with 90 ml of concentrated RBCs for filling the Cytosorb. In the first two days about 4000 ml of ascitic fluid were removed with CVVHDF, and then another 2000 ml removed with permanent peritoneal drainage until the fourth day. After each suspension of use of Cytosorb, a cycle of albumin plasmapheresis was performed for other seven days.
Results
Right after the application of the first Cytosorb Adsorber, about eight hours later, there was a greater respiratory metabolic stability of the patient, a regression of lactates and a normalization of NaHCO3 values. The inothropic weaning began thanks to improved metabolic state and completely stopped within 36 hours. Fenoldopam, Furosemide and Milrinone continuous infusions (Triteted) were maintained longer because the renal function was never recovered. After the second application of Cytosorb the improvement of the pleural effusion was observed and sierositys resolved as well as the improvement of the pulmonary interstitial-alveolar function leading to a rapid reduction of the ventilatory support and FiO2 and successful extubation in the sixth day after the third cytokines apheresis with Cytosorb. At daily physical examination the neurological status improved after discontinuation of the neuroprotective drugs, and the patient showed attention and obeying to command, even if with limitation due to severe osteotendinous and muscle lesions. On the twelfth day the patient was transferred to Nephrology department of the same hospital with a specific pharmacological program and for dialysis treatment due to persistent anuric renal failure.
In the following 72 hours from the transfer, she developed malignant arterial hypertension and posterior reversible encephalopathy syndrome (PRES), heart failure and respiratory failure, so she needed intensive care setting for ventilatory assistance and control of blood pressure with angiotensin-converting-enzyme inhibitor and calcium channel blockers. In addition, an episode of angina occurred requiring enzymatic monitoring and therapy with nitratesTransthoracic critical care echocardiography was used to evaluate biventricular function and complications following acute coronary syndromes: hypertrophic-dilated myocardiopathy was highlighted and controlled by inotropic, lusitropic, and vasodilatory properties of milrinone and levosimendan.
Brain stem MRI was performed showing acute/subacute developmental hemorrhagic foci of posterolateral white and gray matter hemispheres, basal nuclei, brainstem (pons and midbrain) images consistent with posterior reversible encephalopathy (PRES) in addition to the presence of arteritis and narrowing of the arteries of the Polygon of Willis, compatible with the probable presence of the factor Lupus anticoagulants and the development of a picture of diffuse vasculitis and nervous and cardiac involvement during the progression of previously untreated Les. All the necessary pharmacological and depurative support therapies was resumed with a daily cycle of albumin plasmapheresis than scheduled on alternate days meanwhile continuing dialysis for anuria. Corticosteroid treatment with prednisolone was well tolerated and stabilized with a bolus of 0.5 mg/kg/day IV, followed by 50 mg/day through day 7 and progressive tapering during the 2 weeks treatment course up to a fixed dosage of 5 mg/day.
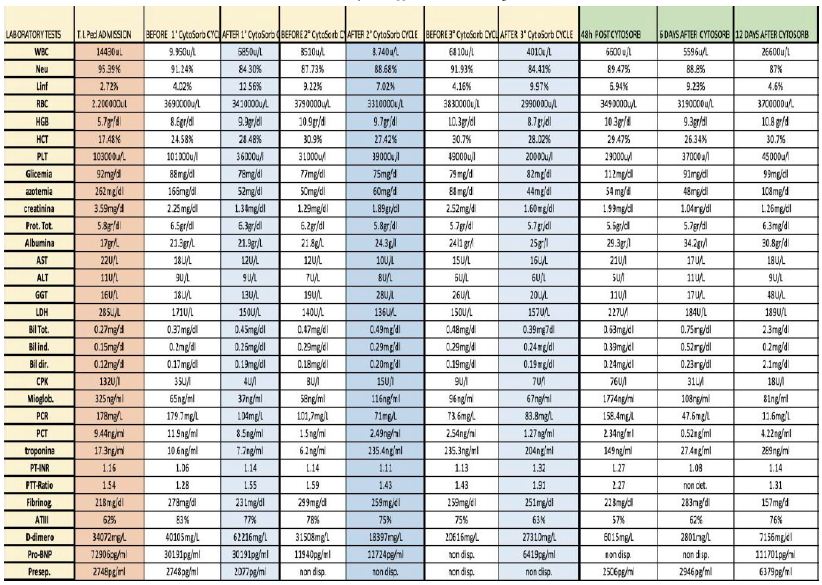
Fortunately, throughout this period of time the patient did not suffer infectious-inflammatory insults, even from the laboratory test point of view Immunosuppressive therapies currently in use was not taken into consideration given the exceptional nature of the case and. The poor clinical state of the patient and mostly because we were not able to find any specific references in the literature treating cases like this. Finally, a single dose of Intravenous Immunoglobulins of 75 mg/kg was administered because a biological fluids (blood, plasma, derivatives of both) administration strategy was preferred in an attempt to accompany, stimulate and regain her spontaneous immunity rather than replace or inhibit it with synthetic and/or semi-synthetic substitutes ( plasma, apheresis ). This therapeutic strategy is very frequent in our group during treatment with MOF sepsi related treated with Cytosorb apply. And it seems to us a well-founded opinion if related to our clinical results already well presented in letterature. Table 5 presents the lab test evolution before and after each single Cytosorb application, 48 hrs after application suspension and at 6 days from the end of Cytosorb application.
Table 5: Cytosorb application lab data timing
The progression of the systemic SLE was completely stopped in ten weeks. We witnessed complete regression of imaging (except for acute evolution of PRES signs) and laboratory parameters, as well as restoration of cardiovascular function with optimal pressure control, complete recovery of neurological status and total functional reactivity, even if paresis of the left upper limb hesitated. At 3 months there was no recovery of renal function consisting in the lupus nephritis picture. The patient, discharged from Intensive Care Unit on March 17th to Nephrology Ward, was then transferred to another hospital for physical rehabilitation on May 31st.
Discussion
The “Rescue Therapy” with compassionate purposes, in a patient in “Imminentia Mortis”, with CytoSorb and cycles of plasmapheresis for uncontrolled macrophage-histocyte activation syndrome (MAS), secondary to infectious trigger evolved in septic state with organ damage, is a consolidated reality. As such, however, the scientific community unconditionally accepts it only in 50% of cases. The majority of patients with pediatric sepsis has favorable outcomes except when sepsis leads to multiple organ dysfunction syndrome (MODS) and the risk death increases in proportion to the number of organs affected. Immune dysregulation is a hallmark of pediatric severe sepsis and MODS, triggered by the uncontrolled and amplified activation of the cytokine cascade leading to prolonged hospitalization and increased late mortality.
Organ dysfunction can be identified as a 2-point variation of the Pediatric Sequential Organ Failure Assessment Score (p-SOFA) assuming that the score is zero in the previously healthy patient, in the absence of comorbidities. A pSOFA score of 2 corresponds to a 10% increased mortality risk in the hospital population with suspected infection associated with organ dysfunction. p-SOFA is computed every day, providing a dynamic assessment of the progression of the disease. It is clear that the further aggravation of organ damage conditions, in the presence of pre-existing dysfunctions, amplifies the severity of state needing the institution of prompt and appropriate treatment.
The initial trigger response of the host is activated by the recognition of a Pathogen Associated Molecular Patterns (PAMPS) or by tissue damage caused by cellular apoptosis and the release of Damage Associated Molecular Patterns (DAMPS). These in turn activate receptors such as the Toll-like receptor and C-type Lectin receptor which, through the activation of Th1 and Th2, activate the cytokine cascade with the release of IL1, IL6 and TNFα. The release of cytokines is trigger for the further activation of numerous pathways of innate and acquired immunity, which results in the migration and activation of macrophages and other cells of the innate immune system, in the release of many others cytokines, chemokines, proteases and reactive oxygen species and amplification of cell damage. The activation of the coagulation system amplified by the notable release of cellular tissue factor and by the imbalance of the anticoagulation system due to protein C deficiency leads, in turn, through the protease activated receptor (PAR’s), resulting in the amplified production and thrombin deposition, to the interruption of the integrity of the endothelial barrier and the Leak Syndrome with tissue edema, dysproteinemia and hypoalbuminemia (and loss of the redox power of the latter). the renin-angiotensin system with increased incidence of renal insufficiency, hyperlactacidemia, cardiovascular instability, respiratory distress.
This condition of SLE has evolved into severe sepsis, favored by a high underlying pathological activity due to the high title of autoantibodies responsible for the exacerbation of organ damage (demonstrated by the high level of ANA and Anti dsDNA and by the low immunoglobulin title of specific immunity and the decrease of C3 and C4, Proteinuria> 3 gr/dl in the urine of 24 h). The meeting point in this state of dysregulation is the initial and final path of the altered innate and acquired immunity during the SLE. In the past, MAS was considered an exclusive complication of rheumatic disease. The progression of SLE in MODS due to the MAS is supported and initiated by a genetic, epigenetic and environmental basis (infections or severe septic state, vitamin D deficiency) which leads to self-persistence of autoantigens and cell damage in the presence of humoral dysregulation with increased cytokines TH1 (IL2), TH2 and TH17 (IL5, IL6, IL21) amplified by the innate immune response and by the self-maintenance of the T cell response and by the production of autoantibodies. The latter is amplified by the increase of INFϒ concentration supported by TNF-dependent factors, through the toll-receptors. The stimulation of B lymphocytes and the uncontrolled macrophage activation with cyclic amplification of the increasing organ damage, is worsened by a break-down of immunological regulation due to TGF-β production and deficit or dysregulation of the TREG/TH17 system.
With an innate substrate of severe immunological dysregulation pathognomonic of SLE, the overlap, as in our case, of the septic trigger with uncontrolled and amplified cytokine cascade aggravating the organ damage and increasing the activity of the disease, was the cause of an abnormal and unstoppable secondary lymphohistocyte-macrophage activation (MAS) which resulted in a serious risk of life for the patient. Rescue therapy with cytokine apheresis through CytoSorb absorber, established early at the onset of organ dysfunction, allowed its reduction with restoration of consciousness, reduction of support and rapid respiratory weaning within 48 hours of treatment with CytoSorb and the reduction until the suspension of the inotropic support at 24 h. There has never been recovery of renal function but only stabilization of renal organ damage with AKI KIDNO SCORE 2 which has attested to dependence on CRRT. The initial calculated pSOFAscore was 13 with an increased risk of mortality of 95% and an APACHE II score of 27 with an estimated non-operative mortality of 55%. Thanks to the Cytosorb treatments, a net reduction in the risk of death was observed: final SOFA calculated equal to 1 with expected mortality lower than 33.3% and an APACHE II calculated equal to 2 with estimated non-operative mortality <4%. The subsequent exacerbation of organ damage at the second admission was controlled with boluses steroid therapy of 500-750 mg/ml for 3 days and subsequent administration of 0.5-1 mg/kg/day subsequently reduced in 2 weeks to 5 mg/day of maintenance in addition to twice a week plasmapheresis. Heavier immunosuppressive therapy with cyclophosphamide or methotrexate and/or azathioprine was contraindicated. Biological immunological therapy with Rituxumab was also evaluated but was not administered due to the worst patient conditions.
Rescue therapy with CytoSorb has been shown to be safe and effective, reducing both the risk of morbidity from 95% to 33% in untreated SLE linked to sepsis and MODS and mortality. Early diagnosis and improved management of SLE significantly increased the probability of survival over the last decade from 5% vs. 95% at 5 years and from 0% vs. 92% at 10 years, from 1995 to 2003. Mortality is essentially linked to disease activity and organ damage as well as bacterial infections that occur in immunosuppressed or immunodeficient patients, as in the case of our patient, subjected to a high dose of glucocorticoids. Immunoapheresis with CytoSorb, in our case, interrupted the self-maintained course of the inflammatory cascade, amplified and mitigated the effects of immunological dysregulation and the imbalance of immune regulation at the basis of SLE, avoiding the progression towards massive lymphohistiocytosis (LHS) and the activation of macrophages (MAS). We await the results of the assay of the cytokines IL6, IL10 and TNFα, before and after each cycle of immunoapheresis performed in another German laboratory, for desirable and precise confirmation of these data.
Conclusion
Immunoapheresis with cytokines has proved effective, in our case, in the treatment of sepsis with organ damage and even more it has been shown to reduce the mortality associated with it, even in the presence of acute and amplified dysregulation of innate immunity. and insufficient and acquired immunological regulation of systemic inflammation as in SLE. It has been shown, as in previous clinical cases, to control uncontrolled lymphohistocytic and macrophage hyperactivation secondary to infectious triggers (MAS). However, further randomized controlled trials in pediatric patients are needed to better frame and define the role of apheresis with CytoSorb as a targeted therapy of amplified systemic inflammation and in the reduction of related organ damage, even more in the context of potent immunological dysregulation. of the acquired and innate immunity, amplified by the septic state.
Author’s Note
The case report of this paper represents a clinical rarity, I would say an exceptionality, since nowadays it has not been found, by us, in the available literature any description of patient like this, suffering from a pathology such as well recognized SLE, has come to medical observation so defied and in so severe clinical state as to require intensive treatment (described in this paper).
References
- Gliwińska A, et al. (2020) A rare complication of systemic lupus erythematosus in a 9-year-old girl: Questions. Pediatr Nephrol. [crossref]
- Leonardo Milella, Maria Teresa Ficarella, Gerolmina Calabresel, Michele Sisto, sorption in Rito Launa Grieco, et al. (2019) Application of Hemoadsorption in Neonatal and Pediatric Hyperinflammatory States:A case Series. American Journal of Pediatrics 5(2): 34.
- Milella Leonardo, Raimondo Pasquale, Ficarella MariaTeresa, Calabrese Gerolmina, Sisto Michele, et al. (2021) Application of combined hemadsorption with eculizumab as rescue treatment of a pediatric patient with multiple organ failure related to severe hemolytic uremic syndrome. J Clin Rev Case Rep 6(8): 718.
- Zhang L, et al. (2022) Continuous renal replacement therapy combined with double filtration plasmapheresis in the treatment of severe lupus complicated by serious bacterial infections in children: A case report. Open Life Sci. [crossref]
- Milella L, Ficarella MT (2017) First application of CVVHDF, Plasmapheresis and “Cytosorb Absorber” to solve Pediatric Haemophagocitic Histyocitosis case. Research in Neonatology and Pediatrics 1.
- LisaMaria Steurer, et al. (2019) Hemadsorption as rescue therapy for patients with multisystem organ failure in pediatric intensive care-Report of two cases reports and review of the literature. Artif Organs. [crossref]
- Leonardo Milella. (2019) Hemoadsorbtion to treate Neonatal and pediatric septic shock and sepsis. World Neonatology and Pediatric Care Meeting 2019.
- L Milella. P RaimondoESA (2020) Hemoadsorption: A promising Rescue Therapy in the Treatment of Critical ill Pediatric Patients. Oral Presentation-European society of Anesthesia.
- Milella Leonardo, Raimondo Pasquale, Ficarella Maria Teresa, Calabrese Gerolmina1, Sisto Michele1 et al. (2021) Hemoadsorption as Bridge to Liver Transplant in A Six-Month Old Patient with Hepatic Failure.Journal of Pediatrics and Neonatology. J Pediatr Neonatol 2(2): 1017.
- Milella, P. Raimondo, N. Lombardi, Maldera M. F. Cito, et al. Hemoadsorption: A Promising Rescue Therapy In The Treatment Of Critical Ill Paediatric Patients.. Conference Paper · May 2020
- Milella L MD, Ficarella MT, MD, Raimondo P MD, Moliterni P MD, Cito F MD, et al. (2016) “Is Cytosorb® a Rescue Therapy in neonatal and pediatric patients?
- Milella, P. Raimondo, N. Lombardi, F. Cito, M.L. Lasorella, MT. Et al. (2019) Hemoadsorption in the rescue treatment of a pediatric patient with MOF related to severe Hemolytic Uremic Syndrome. Bologna 5-6 december 2019
- Scobell, Rebecca (2020) Management of Lupus Nephritis in Children. Indian Pediatr. [crossref]
- Onengiya Harry, et al. (2018) Onset Systemic Lupus Erythematosus: A Review and Update. J Pediatr.[crossref]
- P Srivastava, et al. (2016) Outcome of lupus nephritis in childhood onset SLE in North and Central India: single-centre experience over 25 years. [crossref]
- L Milella (2020) Our experience with Cytosorb in Children and Newborns with Hyperinflammatory states. Ostrawa-News in Pediatric Intensive care.
- Milella Leonardo, Cito Fabiana, Raimondo Pasquale, Ficarella Maria Teresa, Moliterni Paola, et al. (2020) “Our Four Years Experience of Hemoadsorption, Albuminand Heparin Treatment for Paediatric Sepsis: Let’s Give a Chance in Multifactorial Pathological Conditions”. American Journal of Pediatrics 6(3): 207.
- Milella Leonardo1, Cito Fabiana1, Raimondo Pasquale, Ficarella Maria T eresa1, Moliterni Paola, et al. (2021) Our Four Years of Paediatric Sepsis Treatment with Hemoadsorption, Albumin and Heparin: Let’s Give it a Chance in Multifactorial Pathological Conditions. Highlights on Medicine and medical Research 14.
- Vahid Ziaee, et al. (2013) Peripheral gangrene: A rare presentation of systemic lupus erythematosus in a child. Am J Case Rep. [crossref]
- Raimondo P, Ficarella M, Moliterni P, Sisto M, Cito F, Calabrese G, Milella L (2019) Rapid treatment of unexpected septic shock: a single pediatric case recovery for Septic Shock due to Streptococcal Arthritis using early extracorporeal cytokine adsorber treatment. PurificationTherapies-Le idee per la ricerca clinica”-Milano.
- Anadi Mahajan, et al. (2020) Systemic lupus erythematosus, lupus nephritis and end-stage renal disease: a pragmatic review mapping disease severity and progression. Lupus. [crossref]
- Leonardo Milella (2018) Use of CytoSorb in a pediatric case of acute hemorrhagic encephalitis and multiple organ failure. Cytosorb Library. Case of the week.
- Pasquale Raimondo, Maria Teresa Ficarella, Paola Moliterni, Michele Sisto, Fabiana Cito, et al. (2019) Use of CytoSorb in a pediatric patient with septic shock due to streptococcal arthritis. Purification Therapies Workshop – The ideas for clinical research. Milan, Italy March 15-16 2019.
- Milella L (2021) Webinar.“Pediatric use of “Cytosorb”Marijana Matejc –“Cytosorbent”–USA-Stefania magnani,“Aferetica”, Italy.