Abstract
Pulmonary Langerhans Cell Histiocytosis (LCH) in adults is a rare disease and no precise epidemiological data are available concerning its prevalence. Bilateral diffuse nodular infiltration without cystic changes could be one of the Langerhans Cell Histiocytosis (LCH) presentation depend on the stage of evolution of the process. We are reporting in this case an early possible manifestation of LCH that can mimic other wide deferential diagnosis especially among smokers.
Keywords
Smoking related lung disease, Interstial lung disease, Langerhans cell histiocytosis, Smoking
Case Report
58-year-old Irish male with previous medical history of psoriasis, which is controlled on topical treatment, was referred by his GP for Chronic cough and abnormal chest Xray. Patient gave history of chronic dry cough for the last 2 years. No dyspnea or wheezing and his mMRC score was Zero. Review of system was negative for weight loss, hemoptysis, joint pain or night sweat. Significant history of 80 pack-year smoking. Negative exposure to TB or asbestoses.
On examination, his temperature was 36.9°C, his blood pressure was 121/82 mmHg and his oxygen saturation was 97% in room air. There was no evidence of clubbing. No palpable lymphadenopathy. Normal breath sound.
Initial chest Xray showed multiple nodular densities in the both lungs. All his blood tests were normal, including: liver, renal function, calcium, white cell count, hemoglobin, platelet count, Anti-Nuclear Antibody (ANA), Anti-Neutrophil Cytoplasmic Antibodies (ANCA), Erythrocyte sedimentation rate (ESR) and ACE level. Quantiferon was negative.
Pulmonary Function test showed: FEV1: 92% (2.95L), 106% (4.2L), FEV1/FVC: 68%. Lung volumes: RV 116%, TLC 104%. DLCO 82% Kco 88%.
Urgent CT chest (figure 1a) showed: Innumerable predominantly less than 1cm pulmonary nodules in both lungs. The largest nodule in the left lower lobe 7mm.No significant hilar or mediastinal lymph nodes.
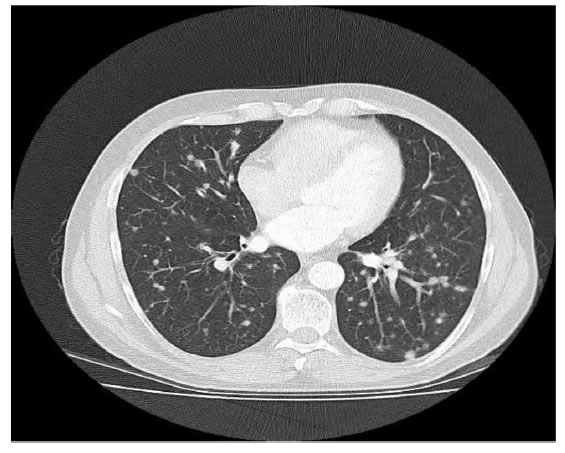
Figure 1a. CT chest View.
Given his extensive smoking history, the likelihood of these abnormalities representing metastatic solid organ malignancy was very high. Other differential diagnoses to be considered include: multiple abscesses, septic emboli, fungal infection, non-inflammatory conditions like sarcoidosis, pneumoconiosis and inflammatory conditions like rheumatoid arthritis.
Bronchoscopy with BAL was done and that was negative for bacterial and MTB culture with normal differentials.
After Respiratory MDM discussion, CT guided biopsy of 7mm nodule in the left lower lobe was done. The core biopsy showed foci of perivascular and peribronchiolar interstitial cellular infiltrate of histiocytic cells with moderate amounts of pale cytoplasm and irregular nuclei. Also present were prominent eosinophils and some small lymphocytes. The large histiocytic cells were strongly positive for S100 and CD1a (figure 1b) and for Langerin confirming the morphological impression of Langerhan’s Cell Histiocytosis.
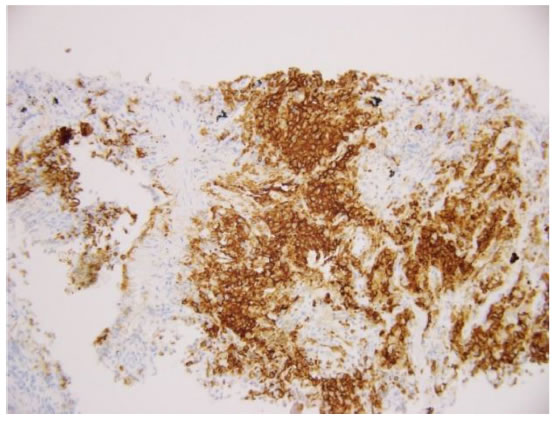
Figure 1b.The histiocytic cells are positive for CD1a which also highlights the perivascular distribution of the infiltrate.
Discussion
Pulmonary LCH in adults is a rare disease and no precise epidemiological data are available concerning its prevalence. Pulmonary involvement with LCH can be observed in patients of any age. Systemic forms of the disease are usually seen in infants and children and pulmonary involvement is often not a prominent feature [1]. In contrast, isolated pulmonary LCH occurs predominantly in young adults with a peak frequency between 20 and 40 years of age. Patients with pulmonary LCH also tend to be heavy smokers [2, 3]. Approximately two thirds of patients present with respiratory symptoms, usually a dry cough, often associated with dyspnea on exertion [4].
The abnormalities seen on the chest radiograph are generally bilateral and symmetrical .More commonly, bilateral widespread cystic lesions may be identifiable.
The most striking characteristic on HRCT of this patient was bilateral diffuse nodular infiltration without cystic changes. That raises another presentation of pulmonary LCH depend on the stage of evolution of the process. Serial studies of individual patients with pulmonary LCH indicate that the lesions evolve as follows: nodules in early stage, cavitary nodules, thick walled cysts then thin walled cysts in late stages [5, 6].
References
- Howarth DM, Gilchrist GS, Mullan BP, et al. (1999) Langerhans cell histiocytosis: diagnosis, natural history, management, and outcome. Cancer 15:2278-2290.
- Crausman RS, Jennings CA, Tuder RM, Ackerson LM, Irvin CG, et al. (1996) Pulmonaryhistiocytosis X: pulmonary function and exercise pathophysiology. Am J RespirCrit Care Med 153:426-435. [Crossref]
- Hance AJ, Basset F, Saumon G, Danel C, Valeyre D, et al. (1986) Smoking and interstitial lung disease.Ann NY AcadSci 465:643-656. [Crossref]
- Schönfeld N, Frank W, Wenig S, Uhrmeister P, Allica E, et al. (1993) Clinical and radiological features, lung function and therapeutic results in pulmonary histiocytosis X. Respiration 60: 38-44. [Crossref]
- Brauner MW, Grenier P, Moeulhi MM,Mompoint D, Lenoir S(1989) Pulmonary histiocytosis X: evaluation with high-resolution CT.Radiology172:255-258. [Crossref]
- Moore ADA, Godwin JD, Müller NL, Naidich DP, Hammar SP, et al. (1989) Pulmonary histiocytosis X: comparison of radiographic and CT findings. Radiology 172:249-254. [Crossref]