We are describing a not yet documented cause for mucopurulent endocervicitis which is triggered by the reaction of neutrophil granulocytes against lactobacilli and is referred to as “lactobacillary endocervicitis” in this contribution. Lactobacilli are a normal component of the vaginal flora.
Samples from 16 women with chronic cervicitis were collected by swabbing the portion. Direct microscopy of the samples showed Gram-positive rods among polymorphonuclear cells (more than 10 per high-power field). Many of the polymorphonuclear cells seemed to try to phagocytize the rods (Figures 1 and 2). All samples tested negative by polymerase chain reaction (PCR) for Chlamydia trachomatis, Neisseria gonorrhoea, Ureaplasma urealyticum, Ureaplasma parvum, M.hominis and M.genitalium. Random samples were also tested for Trichomonas vaginalis and/or human papillomavirus by PCR and resulted negative. None of the women showed signs of bacterial vaginosis. Neither clue cells (by microscopy) nor Gardnerella vaginalis (by culture) were detected in these cases. The 16 observed patients with lactobacillary endocervicitis ranged in age from 25 to 36 years old and 10 were pregnant. In all cases, the cervicitis persisted over 6 weeks and repeated testing for specific agents of infection was performed during that time.
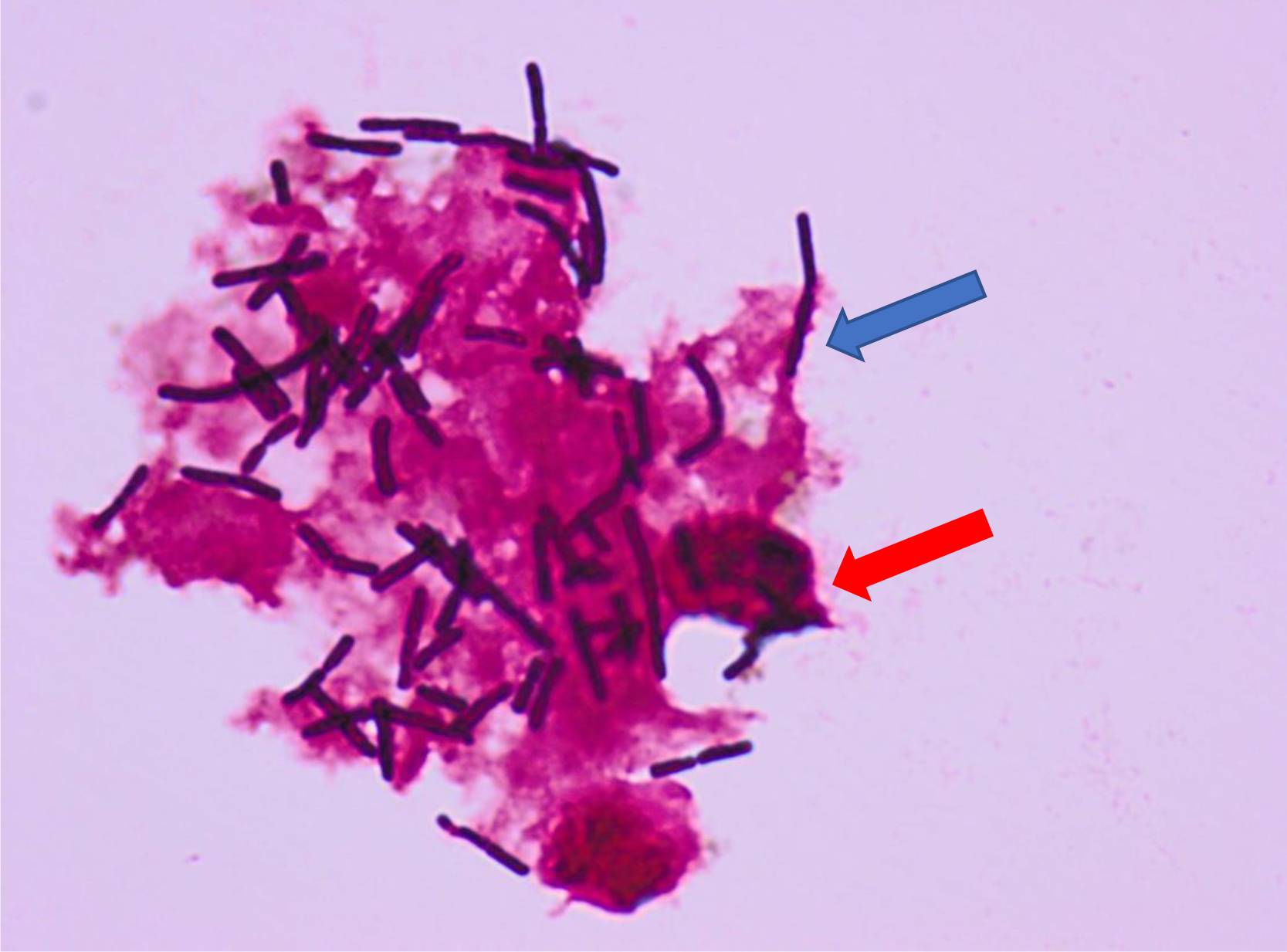
Figure 1. Gram-stain of cervical pus with neutrophils and lactobacilli which are partly phagocytized (red arrow) or captured by the filamentous net (blue arrow) of the neutrophils (high-power field magnification 100 times).
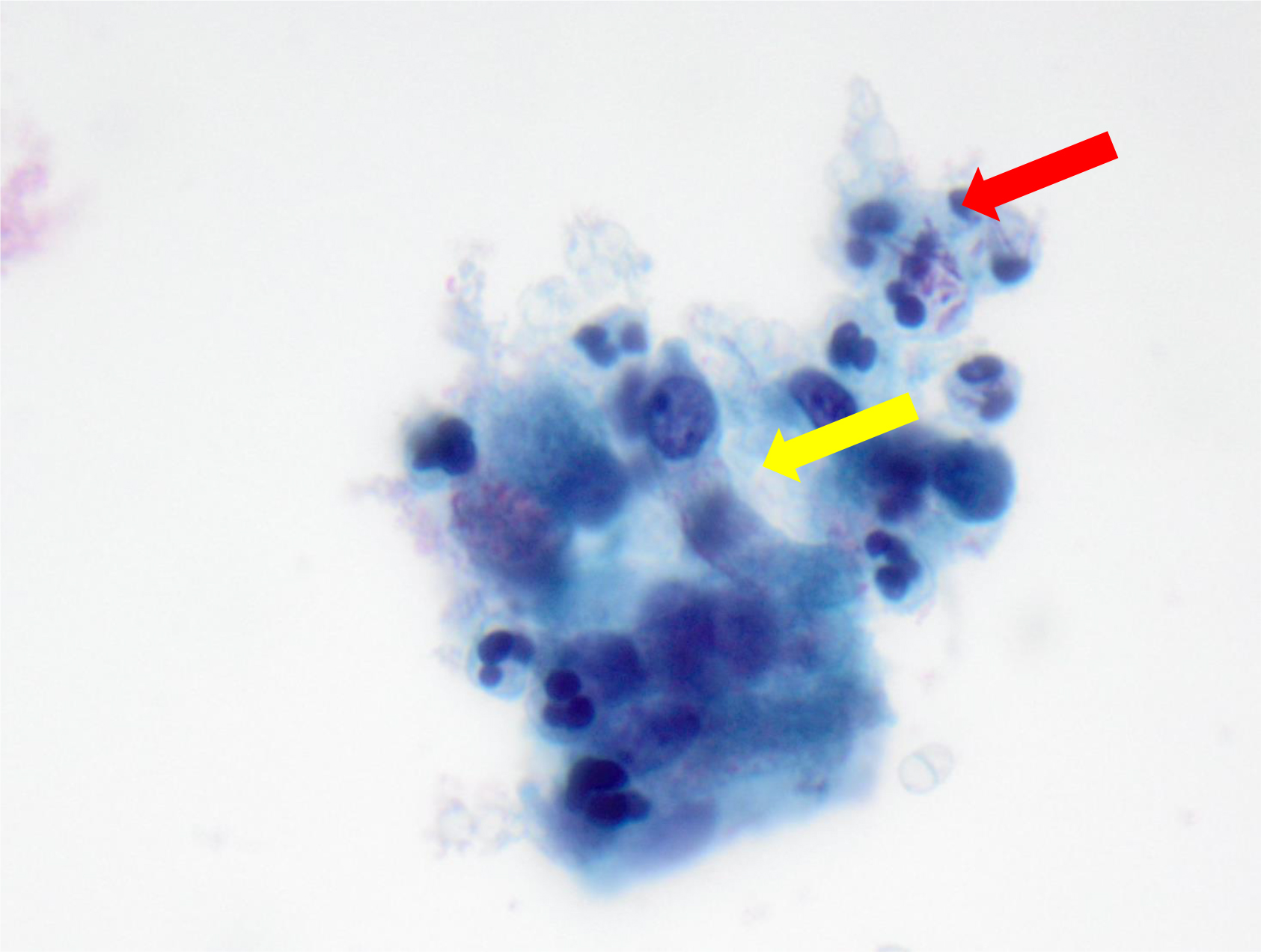
Figure 2. Papanicolau stain of mucous cervical secretion showing columnar cells (yellow arrow) of the endocervix and many neutrophils, some of them with phagocytized lactobacilli (red arrow) (high-power field magnification 60 times).
Chronic cervicitis was first described by Gilbert Strachan in 1929 [1] as the most common lesion seen in the gynaecological practice. The author described gonococci as a possible cause of cervicitis. For other agents of infection, like chlamydia and mycoplasma/ureaplasma, detection techniques were unavailable at the time. Other possible causes for chronic cervicitis are Herpes simplex – virus and Trichomonas vaginalis. About 50% of all diagnosed mucopurulent cervicitis cases are non-specific [2].
Our findings described in this report add another cause for purulent endocervicitis. Lactobacillary endocervicitis is mainly seen in women aged between 25 and 35 years and can become chronic if not treated. Our treatment recommendation was 1g Amoxicillin taken daily orally for 5 to 7 days. In contrast to treatment studies of non-specific purulent endocervicitis [3], our approach proved successful in 15 of our 16 cases. Follow-up investigation of the unresolved case showed the same phagocytized Gram-positive rods in the putrid cervical secretion as observed before Amoxicillin treatment. The lactobacillus in this case was identified by MALDI-TOF as Lactobacillus gasseri and tested sensitive to Ampicillin by Etest (MIC 0.047 mg/L). In another case with successful therapy with Amoxicillin 2 g 1–1-1 for 3 days, the same lactobacilli species was identified in samples taken 1 day before and 69 days after as Lactobacillus johnsonii and Lactobacillus rhamnosus. Amoxicillin tested active against most lactobacilli [4]. Upon completion of antibiotic treatment, preparations containing lactobacilli were locally administered in all cases to re-establish the normal vaginal flora. Our excellent results with the antibiotic therapy described in this report, support our findings that lactobacilli in the wrong place, namely the cervix, can play a role in mucopurulent endocervicitis, which is also often observed in pregnancy.
The pathomechanism of the here described lactobacillary endocervicitis is unclear. A possible explanation might be that there is a constant defence of lactobacilli at the entrance to the endocervix by local defence mechanisms involving neutrophils. If the neutrophil defence is overwhelmed because of changes like pregnancy which impacts the local hormone balance and the opening of the cervix nut mouth , inflammation of the cervix with mucopurulent pus discharge and thus chronic cervicitis can result. Further studies must be performed to shed light on the frequency and importance of lactobacillary infection as a cause of chronic endocervicitis and to establish an optimal treatment regimen.
Acknowledment
We thank Dr. Jäggi Franziska, 4800 Zofingen/Switzerland and her patient for the follow-up samples after treatment.
References
- Gilbert I. Strachan (1929) The Pathology of Chronic Cervicitis. The British Medical Journal 2: 659–661. [crossref]
- Taylor SN, Lensing S, Schwebke J, Lillis R, Mena LA, et al. (2013) Prevalence and treatment outcome of cervicitis of unknown etiology. Sex Transm Dis 40: 379–385. [crossref]
- Lusk MJ, Garden FL, Cumming RG, Rawlinson WD, Naing ZW, et al. (2016) Cervicitis: a prospective observational study of empiric azithromycin treatment in women with cervicitis and non-specific cervicitis. Int J STD AIDS 28: 120–126. [crossref]
- Ocaña V, Silva C, Nader-Macías ME (2006) Antibiotic Susceptibility of Potentially Probiotic Vaginal Lactobacilli Virginia Ocana Clara Silva, and Maria Elena Nader-Macıa. Infect Dis Obstet Gynecol 2006: 18182. [crossref]