Abstract
Introduction: Ridge preservation procedures have been utilized to minimize the alveolar ridge dimensional changes following tooth extraction. This case report describes a novel approach to ridge preservation with an application of a carbon dioxide laser (CO2 laser) to stabilize blood clot formation and stimulate wound healing.
Case presentation: A 76-year-old Caucasian male with history of type 2 diabetes was referred for extraction of #8 and placement of a dental implant to reconstruct the area. Extraction was performed in a minimal traumatic manner and a mineralized freeze-dried bone allograft was placed in the socket. A 10,600 nm wavelength CO2 laser was used in setting of 1.0 watts focused continuous wave energy to stabilize the blood clot over the extraction site. The laser was used until a char layer was formed. This char layer was a non-bleeding stable blood clot, and the end-point of laser application was set as “no blood flow from the clot are within 10 seconds.” No membranes or sutures were used. Eleven weeks after the extraction and ridge preservation, a 4.1x10mm dental implant was placed with >35N/cm of primary stability and Implant stability quotient (ISQ) value of 83. A provisional crown was delivered at the time of implant placement. Three months following implant placement, the final restoration was delivered. The soft and hard tissue healing were uneventful to achieve esthetic and functional outcomes.
Conclusion: Within limits of this case report, the application of CO2 laser for “Laser-Assisted Blood Clot Formation” may enhance the soft and hard tissue healing following extraction for ridge preservations.
Keywords
Carbon Dioxide Laser, Ridge Preservation, Implant, Immediate Provisional
Introduction
Ridge preservation procedures have been utilized to minimize the loss of alveolar ridge dimension following extractions [1,2]. One of the most commonly used methods is application of bone substitutes graft materials into the extraction sockets as a scaffold for space maintenance and new bone formation since bundle bone will be resorbed following extractions [3–5]. Several studies have shown the positive effect on extraction site healing with laser irradiation [6,7]. Fukuoka reported that carbon dioxide laser irradiation in rat extraction sites resulted in less concavity and lower vertical alveolar ridge reduction compared to non-irradiated sites [8]. Moreover, histo-immunostaining revealed that less myofibroblastic activity was noted in irradiated areas. In other words, less wound contraction was noted due to the blood clot stability and possible low-level laser therapy (LLLT) effects [8]. A carbon dioxide laser (CO2 laser: wave length:10,600µm) has been utilized in dentistry primarily for soft tissue and hemostasis procedures [9]. Application of CO2 laser is considered relatively safer because the energy is absorbed on the surface of water and causes less scatter. The CO2 laser is used in a non-contact manner which is beneficial to stimulate the blood clot compared to other types of lasers which need direct contact on the tissues [10]. The aim of this case report is to demonstrate the novel application of CO2 laser for alveolar ridge preservation procedures.
Clinical Presentation
A 76-year-old white male presented to Indiana University School of Dentistry Graduate Periodontics Clinic for consultation for an implant of #8 in November 2017. The patient’s chief complaint was “This crown keeps falling out and needs to be fixed”. The patient’s medical history revealed well-controlled Type 2 diabetes (HbA1c:6.2%), hypertension, and history of myocardial infarction (stent and bypass surgery). His medications included clopiogrel 75mg and aspirin 81mg. The patient also reported that he took levothyroxine for hypothyroidism medication and used a CPAP machine for sleep apnea. #8 was deemed to be non-restorable due to recurrent caries. Treatment options were discussed with patient and #8 extraction and subsequent implant placement was chosen (Figure 1, 2).

Figure 1. Pre-operative Clinical Appearance.

Figure 2. Pre-operative Periapical Radiograph.
Case Management
Following the local anesthesia administration, the crown and post were removed. A sulcular incision was made around the root to sever the supracrestal attached tissue. No flap reflection was performed. The remained root was sectioned, elevated and extracted with periotome elevators. After granulation tissue removal, a 2–3 mm fenestration was noted on the facial mid to apical third of the extraction site. Mineralized freeze-dried bone allograft (FDBA)† was hydrated with saline and placed in the extraction site to the level of the crestal bone. A 10,600 nm wavelength CO2 laser‡ was used at a setting of 1.0 watts focused continuous wave energy to stabilize the blood clot over the extraction site. A gold tip was attached to the laser hand-piece. Target distance was set approximate 10mm from the edge of the gold tip. The divergence of beam was 6.2 degree and the spot size at the target was Ø0.48mm. Since we utilized 1W focused continuous wave mode of this device, the power density was 555.6W/cm2. A CO2 laser is absorbed by water, and it does not penetrate into the deep layer of the soft and hard tissue. However the careful attention was taken to keep moving the laser tip to reduce the heat generation and avoid the direct application onto the hard tissue structure including teeth and alveolar bone surfaces. The laser tip was moved continuously with circle motion approximately 3–5 turns/sec over the extraction site. Extraction site is approximately 10mm diameter, so beam movement is 9.4–15.7cm/sec of speed. This movement can reduce the concentration of energy on the one spot which increase the temperature. The laser was used until a char layer was formed. This char layer was a non-bleeding stable blood clot, and the end-point of laser application was set as “no blood flow from the clot are within 10 seconds” (Figure 3–5).
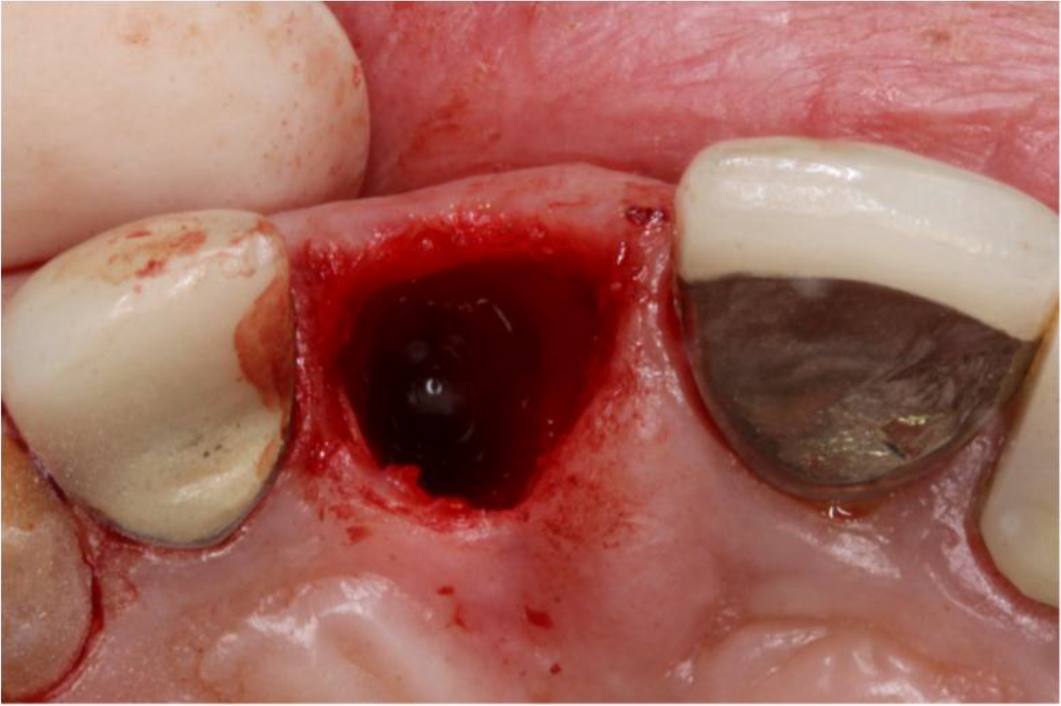
Figure 3. Immediately after the extraction: Buccal bone was present.

Figure 4. Description of laser tip and object.

Figure 5. Laser Assisted Blood Clot Formation and Stabilization were achieved.
Results
The wound healing was uneventful and no complications were noted. The patient returned for 1, 3 and 7 week post-operative visits (Figure 6–8). At 11 weeks following the extraction, the site was re-entered for implant placement. Following crestal and slight vertical incision on mesial on #8, a full thickness flap was elevated. Crestal bone revealed solid and flat alveolar bone upon flap reflection in the former extraction site although slight soft tissue concavity was noted. The buccal-palatal dimension ofalveolar bone was sufficient for the planned dental implant. Implant osteotomy was performed per manufacturer recommendation and a 4.1 x 10 mm implant§ was placed with an insertion torque of 35 N/cm. Implant Stability Quotient (ISQ) value‖ showed 83 from both buccal and lingual directions. Due to the high implant stability, an immediate provisional was fabricated chairside and delivered (Figure 9–13). The use of an immediate provisional allowed better soft tissue emergence profile as well as patient comfort and convenience. Three months following implant placement, a definitive restoration was delivered. Final restoration showed good soft tissue esthetics and papillary fill, and the outcome has been stable up to one year (Figure 14,15).

Figure 6. 1 week post-operative clinical view.

Figure 7. 3 weeks post-operative clinical view.

Figure 8. 7 weeks post-operative clinical view.

Figure 9. 11 weeks post-operative clinical view.
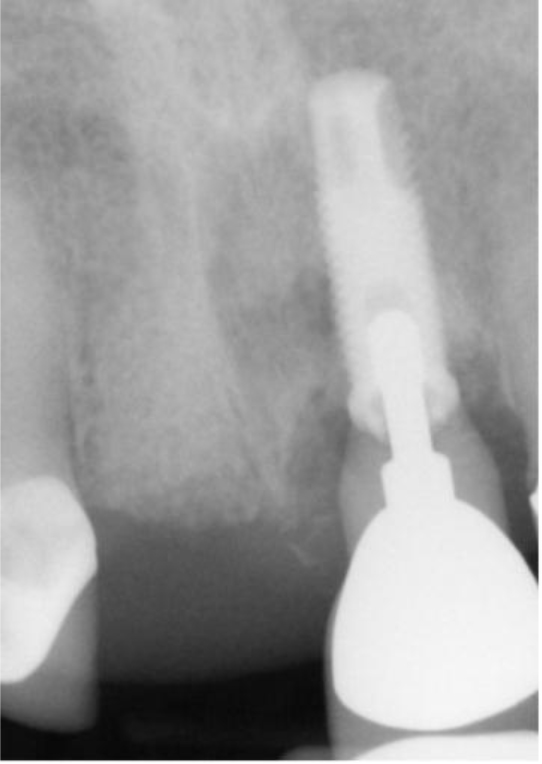
Figure 10. 11 weeks post-operative periapical radiograph.
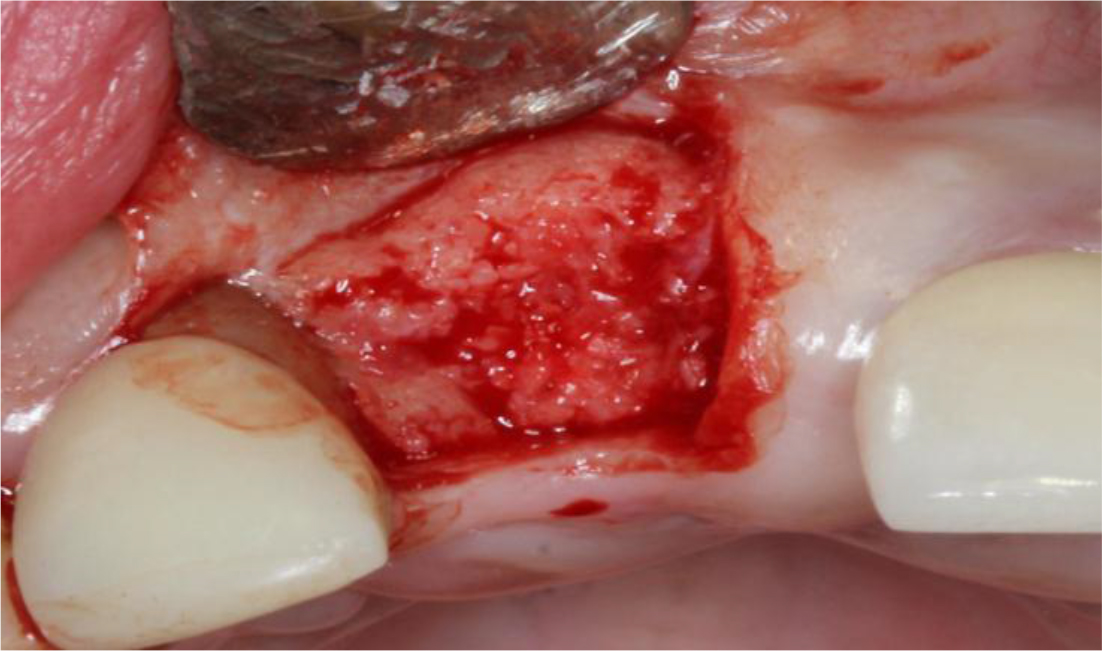
Figure 11. Bone regeneration was noted 11 weeks after the extraction.

Figure 12. 1 week after the implant placement and provisional crown delivery. (Clinical)
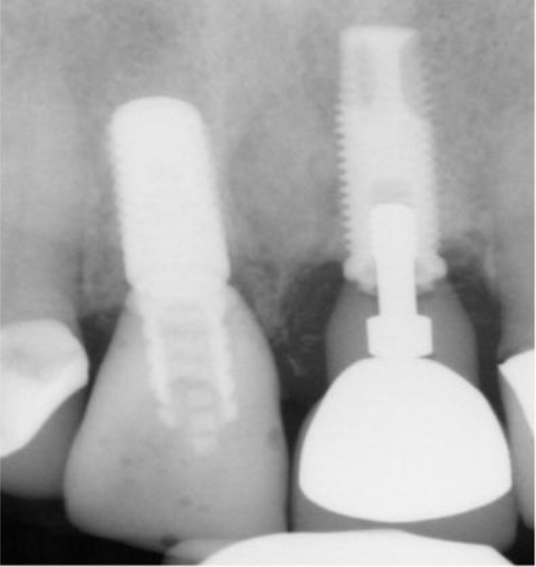
Figure 13. 1 week after the implant placement and provisional crown delivery. (Periapical radiograph)

Figure 14. 1 year after the implant placement with the final crown: Acceptable papillae fill and gingival health was obtained
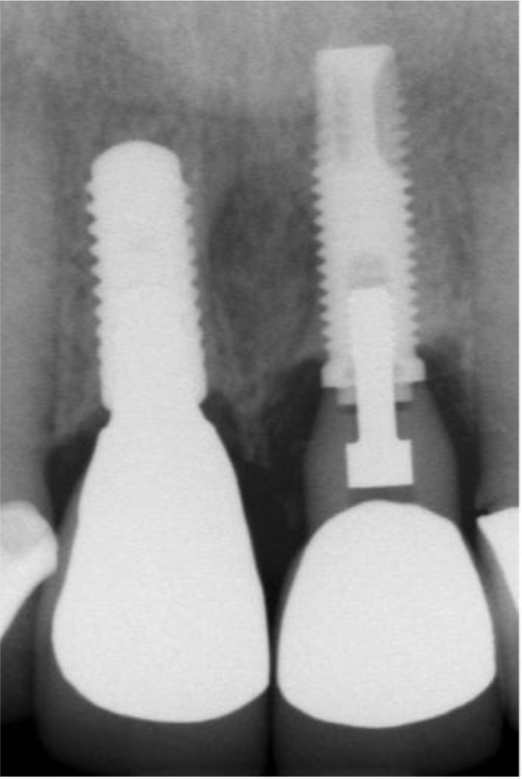
Figure 15. 1 year after the implant placement with the final crown: No marginal bone loss was noted.
Discussion
Extraction sites usually heal by secondary intention, and slight concavity over the crestal area is very common [11]. Amler described the healing process of human extraction wounds [12]. For the undisturbed healing sites, initial blood clot formation fills the entire socket and followed by immature connective tissue formation and epithelization over the wound. Disruption of the blood clot during healing can result in disturbance of the normal healing pattern and is suspected to be the cause of ofalveolar osteitis. The exposed alveolar bone surface causes not only pain also significant wound healing delayed. According to this description, blood clot stability will directly affect the wound stability which can maximize the regenerative capacity. Cortellini and Tonetti compared application of modified minimal invasive surgery with or without graft materials or growth factors [13]. Then the study showed that there were no statistical differences between groups. The key to achieve the maximum potential of regenerative outcome is to create a stable environment for soft and hard tissue healing. In this case report, we tested the application of CO2 laser to stabilize the blood clot formation over the extraction site. Due to the blood clot stability, relatively faster epithelization over the extraction site was observed during the initial healing process. Meloni et al. utilized a porcine collagen matrix and connective tissue graft to cover the extraction site following placement of a bone graft substitute. Both methods did not show any significant differences for healing outcomes. The concept of those procedures was also to achieve wound stability by placing graft materials. Disadvantages of those soft tissue grafts and those substitutes are required to place sutures to obtain stabilization. In addition to those sutures, harvesting of connective tissue requires a secondary surgical site, and those substitutes are not cost friendly [14]. On the contrary, utilization of CO2 laser does not require any sutures nor additional soft grafts since this technique is simply stimulating blood coagulation and stabilizing the blood clot. The authors would like to propose that this procedure can be named as a “laser assisted blood clot formation”. However, there is currently no evidence to show how soft tissue healing process with CO2 laser can induce the bone maturation and preservation of ridge dimension. Due to the nature of case report, the other limitation of this study was that ridge dimension change was not measured prospectively. Although the existing buccal bone thickness was thin at the time of extraction, this case cannot prove which factor (bone substitute grafting or blood clot stability with CO2 laser) contributed to the outcome of this case report. Further studies are needed to substantiate these results.
Conclusion
Within limits of this case report, the application of CO2 laser for “Laser-Assisted Blood Clot Formation” may enhance the soft and hard tissue healing following extraction for ridge preservations.
Acknowledgement
The authors would like to acknowledge Dr. Eiji Funakosi, Private practitioner, founder of Funakoshi Research Institute of Clinical Periodontology, Fukuoka, Japan for the assistance to develop this laser protocol.
The authors also would like to acknowledge Mr. Tatsuya Kashima and Mr. Wataru Kikuchi (THE YOSHIDA DENTAL MFG. CO., LTD) for the calculation of the total energy of this laser application.
References
- Hämmerle CH, Araújo MG, Simion M; Osteology Consensus Group 2011 (2012) Evidence-based knowledge on the biology and treatment of extraction sockets. Clin Oral Implants Res 5: 80–82. [crossref]
- Schropp L, Wenzel A, Kostopoulos L, Karring T (2003) Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 23: 313–323.
- Araujo MG, Lindhe J (2005) Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 32: 212–218.
- Frost NA, Banjar AA, Galloway PB, Huynh-Ba G, Mealey BL (2014) The decision-making process for ridge preservation procedures after tooth extraction. Clinical Advances in Periodontics 4: 56–63.
- De Risi V, Clementini M, Vittorini G, Mannocci A, De Sanctis M (2015) Alveolar ridge preservation techniques: a systematic review and meta-analysis of histological and histomorphometrical data. Clin Oral Implants Res 26: 50–68.
- Brawn PR, Kwong-Hing A (2007) Histologic comparison of light emitting diode phototherapy-treated hydroxyapatite-grafted extraction sockets: a same-mouth case study. Implant Dent 16: 204–211.
- Cranska J (2008) Post-extraction laser hemostasis with immediate insertion of a bonded bridge. Dent Today 27: 108–110.
- Fukuoka H, Daigo Y, Enoki N, Taniguchi K, Sato H (2011) Influence of carbon dioxide laser irradiation on the healing process of extraction sockets. Acta Odontol Scand 69: 33–40. [crossref]
- Cobb CM (2006) Lasers in periodontics: a review of the literature. J Periodontol 77: 545–564. [crossref]
- Aoki A, Mizutani K, Schwarz F (2015) Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000 68: 217–269.
- Lin Z, Rios HF, Volk SL, Sugai JV, Jin Q, et al. (2011) Gene expression dynamics during bone healing and osseointegration. J Periodontol 82: 1007–1017. [crossref]
- Amler MH (1969) The time sequence of tissue regeneration in human extraction wounds. Oral Surg Oral Med Oral Pathol 27: 309–318. [crossref]
- Cortellini P, Tonetti MS (2011) Clinical and radiographic outcomes of the modified minimally invasive surgical technique with and without regenerative materials: a randomized-controlled trial in intra-bony defects. J Clin Periodontol 38: 365–373.
- Meloni SM, Tallarico M, Lolli FM, Deledda A, Pisano M, et al. (2015) Postextraction socket preservation using epithelial connective tissue graft vs porcine collagen matrix. 1-year results of a randomised controlled trial. Eur J Oral Implantol 8: 39–48.