Abstract
Aim: The impact of the global COVID-19 on colorectal conditions remains unknown. Thus, we aimed to determine the effect of COVID-19 limitations on diverticular disease.
Method: Retrospective analysis of Premier hospital inpatient files from 1/1/2019 through 6/30/2020 for admissions and surgical procedures for patients with diverticular disease. Comparison between first six months of 2019 and 2020 for disease incidence, severity, operative management, and adverse events. Primary outcome measure was pulmonary failure and secondary outcome measures were adverse events, rates of hospitalization and surgical intervention.
Results: Admissions for diverticulitis declined by 25% in 2020 as compared to 2019. The proportion of urgent diverticular disease cases rose significantly in April 2020 to 59.1% from an average of 37.5% in 2019 (p<0.0001). Although diverticular abscess comprised 55.1% of all admissions in 2019, the proportion of abscess cases rose to 69.3% in April 2020. Consequently, 38% of all procedures in the spring of 2020 resulted in a stoma, 29% higher than in 2019. Select postoperative complications including organ space infections and sepsis were significantly higher in April 2020. Most importantly, pneumonia complications were similar in 2019 (1.6%) and 2020 (1.8%) (p=0.5) as were respiratory failure rates (4.2% in both 2019 and 2020).
Conclusions: During the COVID-19 pandemic, there was a notable decreased rate of hospitalization for diverticulitis but an increased disease severity among those admitted. The increase in diverticular abscess procedures coincided with higher rates of organ space infections and ostomy creations but no difference in respiratory complications. These data indicate that surgery for diverticulitis in the setting of the COVID-19 pandemic can be safely performed.
Statement: Limitations incited by the COVID-19 pandemic resulted in decreased hospitalization rates for diverticulitis but increased severity of disease for those admitted, which coincided with increased rates of postoperative organ space infections and ostomy creations. However, respiratory complications remained stable demonstrating continued safety of operative management in this critical time.
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Although COVID-19 has a variable clinical course, the virus is associated with severe respiratory, vascular, and/or gastrointestinal symptoms which can progress in severity in high‐risk individuals. In the most common case, COVID-19 is characterized by symptoms of viral pneumonia such as fever, fatigue, and dry cough [1]. The virus is highly contagious as it is spread from person to person through respiratory secretions and/or contaminated fomites. Within short order, Coronavirus spread around the world leading the World Health Organization to declare COVID-19 a pandemic on March 11, 2020 [2].
The COVID-19 pandemic changed many dimensions of health care in the United States and affected the operations of a host of healthcare facilities in 2020 [3]. In surgery, the American College of Surgeons recommended that “each hospital, health system, and surgeon should thoughtfully review all scheduled elective procedures with a plan to minimize, postpone, or cancel electively scheduled operations, endoscopies, or other invasive procedures until we have passed the predicted inflection point in the exposure graph and can be confident that our health care infrastructure can support a potentially rapid and overwhelming uptick in critical patient care needs.” These recommendations led to reduced numbers of patients in ambulatory clinics, fewer screening and other elective procedures, as well as other interruptions in inpatient services [4,5]. Models of these interruptions in cancer screening and treatment have predicted over 10,000 excess deaths from breast and colorectal cancer over the next decade [6].
Given the limitations and restrictions in surgical care as well as other concerns related to obtaining non COVID-19 related treatment, we undertook a study to determine the impact of COVID-19 on colorectal surgery care in the United States. In particular we sought to evaluate diverticulitis care during the height of the pandemic as well as outcomes from surgery during the height of the pandemic as compared to one year prior. In addition, we evaluated the risk of respiratory complications related to surgery during the COVID-19 pandemic, as well as all other postoperative complications, as compared to one year earlier. These data are of particular importance as other COVID surges occur as well as other potential respiratory epidemics.
Methods
Database
We abstracted records from the Premier hospital inpatient files from 1/1/2019 through 6/30/2020 accounting for 586 hospitals. The Premier Healthcare Database is one of the most comprehensive electronic healthcare databases originating from the merger of Premier with American Healthcare Systems and SunHealth in 1997 [7]. Data derive from a large, U.S. hospital-based, service-level, all-payer capture model that contains information on inpatient discharges, primarily from geographically diverse non-profit, non-governmental and community and teaching hospitals and health systems from rural and urban areas [7]. Hospitals and healthcare systems submit administrative, healthcare utilization and financial data from patient encounters approximating 10 million inpatient visits per year or twenty-five percent of annual United States inpatient admissions. The data are de-identified and HIPAA compliant, thereby considered exempt from Institutional Review Board oversight as dictated by Title 45 Code of Federal Regulations, Part 46 of the United States, specifically 45 CFR 46.101(b).
Cohort
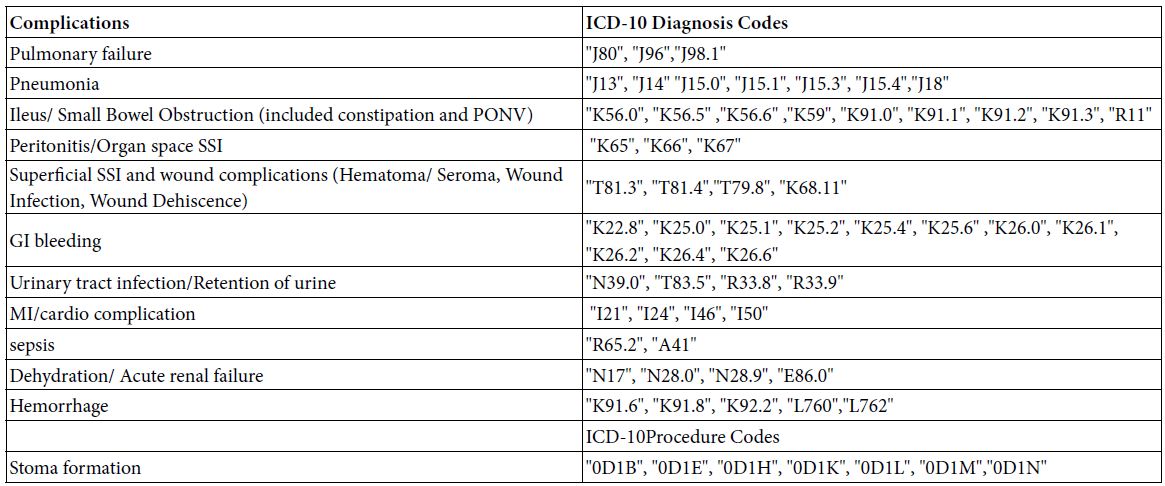
All adult patients with diverticular disease were identified based on the primary diagnosis with ICD-10 codes of K57.20, K57.21, K57.32 or K57.33 for hospitalization. Patient demographics were collected as covariates including race, sex, age, and marital status. Charlson comorbidity score was also calculated and can be calculated as described in previous publications [8]. In addition, the covariates of payer information, hospital regional location, hospital rural urban location, hospital bed size, and teaching status of hospital were also abstracted. Presence of abscess at time of admission was determined based on patients who had ICD-10 diagnosis codes K57.20 or K57.21. Patients were then assigned as either medical or surgical based on having surgical Disease Related Group (DRG) codes and ICD-10 procedure codes (Appendix 1). Minimally invasive procedures were identified with the ICD-10 surgical procedure codes possessing the 5th digit as 3, 4 or 6 while open procedures were identified with the ICD-10 surgical procedure codes possessing the 5th digit as 0. Formation of stoma was identified based on ICD-10 procedure codes listed in appendix 1. Cases were classified as urgent cases by hospital admission type.
Primary Outcome
The outcome of primary interest was respiratory failure defined with hypoxia or hypercapnia during the index hospital stay and identified with ICD-10 diagnostic codes of J80, J96, or J98.1 (Appendix 1).
Secondary Outcomes
Secondary outcomes of interest include pneumonia as recorded by ICD-10 codes (see Appendix 1). Additionally, we recorded adverse events of ileus/small bowel obstruction, peritonitis/organ space infection, superficial surgical site infection, gastrointestinal bleeding, urinary tract infection, myocardial infarction, sepsis, acute renal failure, and hemorrhage complications. A full list of ICD-10 codes is included in appendix 1.
Analysis
Admissions and surgical procedures for patients with diverticular disease were compared for the first six months of 2019 (1/1/2019 through 6/30/2019) as compared to the first six months of 2020 (1/1/2020 through 6/30/2020) during the COVID-19 pandemic. Patient demographics, patient covariates, use of surgery procedures, presence of abscess, and adverse events were compared during the two periods with Chi square analysis for categorical variables. Analysis was performed at the monthly basis for admissions and outcomes. In addition, we compared the development of respiratory complications such as pneumonia or pulmonary failure during the two time periods with the same analysis. Multivariable logistic regression analyses were performed to control for urgent nature of surgery while evaluating postoperative complications. The multivariable analysis only included use of urgent nature of surgery and not additional variables due to the small sample size. All analyses were performed with SAS 9.4 and p value of less than 0.05 was considered significant based on multiple tests of variance.
Results
Cohort
Admissions for diverticulitis for the first six months of 2019 totaled 20,717 patients with 14,408 (69.6%) medical admissions and 6,309 (30.5%) surgical admissions. However, during the first six months of 2020, there were 24.6% fewer total admissions comprising 15,630 total admissions with 10,829 (69.2%) medical admissions and 4,801 (30.7%) surgical admissions. Patient demographics were similar across time periods. There were proportionately more women admitted during each time period. In addition, there were proportionately more patients over age 65 and with Charlson Comorbidity of 0 regardless of time period. Commercial insurers were the most common payer for both time periods and most patients were treated at hospitals with over 500 beds (Table 1).
Table 1: Patient and hospital characteristics.
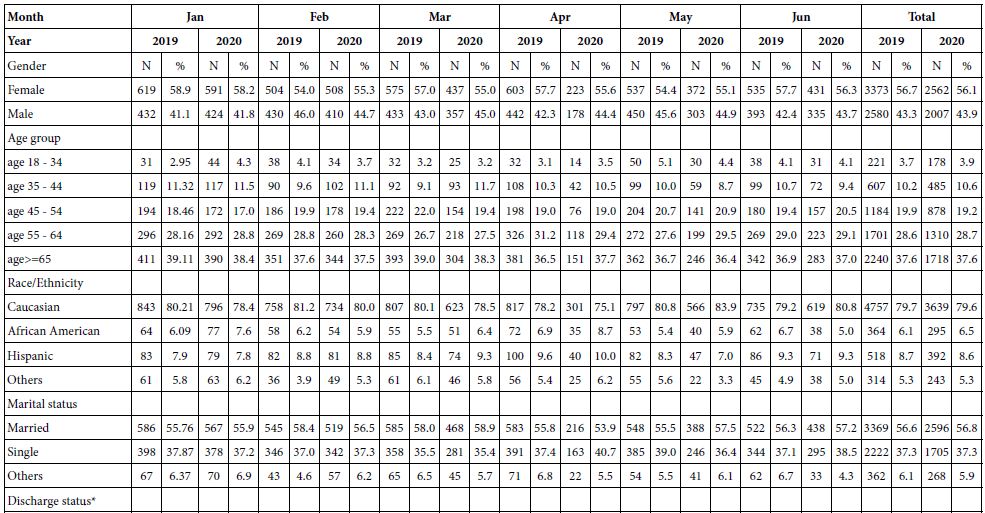
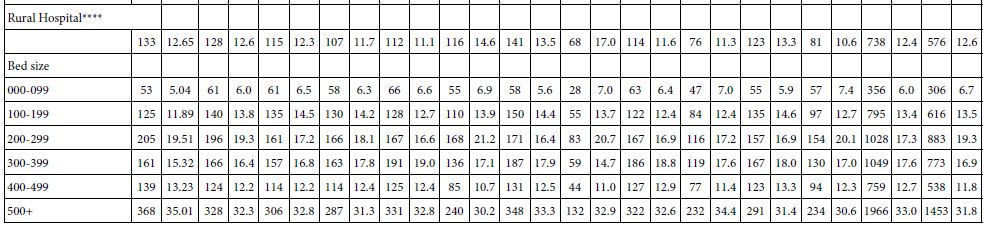
Chi-square analysis was used to compare difference in each characteristic between the years 2019 and 2020 within each month. All p >0.05, except: *p=0.0114 and 0.0036 in April and May respectively; **p=0.0002 in April; ***p=0.024 in April and ****p=0.0266 in March. All cells less than 10 were marked as “<10” and their corresponding percentages were not reported (NR). CCI: Charlson Comorbidity Index.
Disease Severity
There were proportionately more patients admitted with diverticular abscess in the first six months of 2020 as compared to the same time period in 2019 (p<0.0001). There were 9,872 patients (47.7%) admitted with diverticular abscess in 2019 as compared to 7,860 patients (50.3%) in 2020 (Table 2).
Table 2: Incidence of diverticular abscess among all hospital admissions.
| Year |
2019 |
2020 |
|
||
| Months |
N |
% | N | % |
p-value |
| Jan |
1646 |
48.0 | 1615 | 48.4 |
0.6934 |
| Feb |
1537 |
48.5 | 1558 | 49.0 |
0.6771 |
| Mar |
1671 |
47.3 | 1330 | 49.9 |
0.0416 |
| Apr |
1670 |
47.6 | 917 | 54.6 |
<.0001 |
| May |
1715 |
47.8 | 1148 | 51.0 |
0.0173 |
| Jun |
1633 |
47.0 | 1292 | 51.4 |
0.0008 |
| Total |
9872 |
47.7 | 7860 | 50.3 |
<.0001 |
The number of urgent surgical cases for diverticular disease was 2,123 for the first six months of 2019 or 33.7% of surgical cases. However, the number of urgent cases in the first six months of 2020 was 1,756 or 36.6% of surgical cases (p<0.001). Comparing individual months of both calendar years, there were proportionately more urgent cases in April 2020 (59.2%) as compared to 36.9% in April 2019 (p<0.0001). There were no other significant differences in urgent surgical cases by month for the other months (Table 3).
Table 3: Urgent Operations by Month.
| Year |
2019 |
2020 |
|
||
| Months |
N |
% | N | % |
p-value |
| Jan |
360 |
34.3 | 336 | 33.1 |
0.5805 |
| Feb |
322 |
34.5 | 326 | 35.5 |
0.64 |
| Mar |
365 |
36.2 | 322 | 40.6 |
0.0595 |
| Apr |
392 |
37.5 | 237 | 59.1 |
<.0001 |
| May |
360 |
36.5 | 285 | 42.2 |
0.0182 |
| Jun |
324 |
34.9 | 250 | 32.6 |
0.3245 |
| Total |
2123 |
35.7 | 1756 | 38.4 |
0.0035 |
Surgery
When surgery was performed in 2019, 55.1% had a diverticular abscess yet 58.6% had an abscess during the same time period in 2020 (p=0.004). In April of 2020, there were substantially more surgical patients with diverticular abscess (69.3%) then in the same time period in 2019 (55.6%) (p<0.0001) (Table 4). In addition, minimally invasive surgical treatment for diverticular disease was slightly less common in 2019 (41.9%) as compared to 2020 (42.8%). The most significant difference in use of minimally invasive procedures occurred in April at which time minimally invasive procedures were used in 43% of all procedures in 2019, yet only 34% of cases in April 2020 (p<0.004) (Table 4).
Table 4: Abscess rate and surgical approach among patients who underwent surgery.
| 2019 | 2020 | |||||
| N | % | N | % |
p-value |
||
| Abscess |
Jan |
590 | 56.1 | 558 | 55.0 | 0.5953 |
| Feb | 509 | 54.5 | 504 | 54.9 |
0.8610 |
|
|
Mar |
543 | 53.9 | 463 | 58.3 | 0.0593 | |
| Apr | 581 | 55.6 | 278 | 69.3 |
<.0001 |
|
|
May |
551 | 55.8 | 400 | 59.3 | 0.1647 | |
| Jun | 509 | 54.9 | 447 | 58.4 |
0.1475 |
|
|
Total |
3283 | 55.1 | 2650 | 58.0 |
0.0035 |
|
| MIS |
Jan |
465 | 44.2 | 430 | 42.4 | 0.3889 |
| Feb | 393 | 42.1 | 415 | 45.2 |
0.1745 |
|
|
Mar |
451 | 44.7 | 339 | 42.7 | 0.3846 | |
| Apr | 449 | 43.0 | 138 | 34.4 |
0.003 |
|
|
May |
401 | 40.6 | 248 | 36.7 | 0.1106 | |
| Jun | 389 | 41.9 | 346 | 45.2 |
0.179 |
|
|
Total |
2548 | 42.8 | 1916 | 41.9 |
0.3723 |
|
| Stoma Creation |
Jan |
281 | 26.7 | 284 | 28.0 |
0.5260 |
|
Feb |
255 | 27.3 | 262 | 28.5 | 0.5525 | |
| Mar | 291 | 28.9 | 278 | 35.0 |
0.0053 |
|
|
Apr |
321 | 30.7 | 176 | 43.9 | <.0001 | |
| May | 287 | 29.1 | 241 | 35.7 |
0.0044 |
|
|
Jun |
265 | 28.6 | 207 | 27.0 | 0.4838 | |
| Total | 1700 | 28.6 | 1448 | 31.7 |
0.0005 |
MIS: Minimally Invasive Surgery.
A stoma was made in 28.6% of all patients who underwent surgery during 2019. Yet in 2020, there was a substantially greater proportion of stomas fashioned (31.7% of all surgical procedures; p=0.0005). In April of 2020, the proportion of patients who received a stoma reached 43.9% which was substantially higher (30.7%) than in April of 2019 (p<0.0001) (Table 4).
Respiratory Adverse Events
Most importantly, pneumonia complications were similar in 2019 (1.7%) as they were in 2020 (1.8%) (p=0.5). There was no difference in pneumonia rates by month across time periods. In addition, respiratory failure rates were similar across time periods, 4.2% in 2019 and 2020, with the only significant difference occurring in April (4.2% in 2019 vs 6.8% in 2020). Rates of respiratory failure were higher in patients who had urgent surgery and no different even in April of 2020 (10.1%) as compared to April 2019 (7.9%) (p=0.4) (Table 6).
Table 6: Postoperative respiratory adverse events.
| Year |
2019 |
2020 |
|
||
| Month |
N |
% | N | % |
p-value |
| Pneumonia | |||||
| Jan |
15 |
1.4 | 23 | 2.2 |
0.156 |
| Feb |
20 |
2.2 | 20 | 2.2 |
0.9559 |
| Mar |
22 |
2.2 | 18 | 2.2 |
0.9038 |
| Apr |
14 |
1.4 | <10 | NR |
0.8896 |
| May |
15 |
1.6 | <10 | NR |
0.7544 |
| Jun |
12 |
1.2 | <10 | NR |
0.6371 |
| Total |
98 |
1.7 | 83 | 1.8 |
0.5053 |
| Pulmonary failure | |||||
| Jan |
51 |
4.8 | 45 | 4.4 |
0.651 |
| Feb |
36 |
3.8 | 44 | 4.8 |
0.3205 |
| Mar |
37 |
3.6 | 29 | 3.6 |
0.9837 |
| Apr |
43 |
4.2 | 27 | 6.8 |
0.0378 |
| May |
37 |
3.8 | 19 | 2.8 |
0.3001 |
| Jun |
44 |
4.8 | 28 | 3.6 |
0.2701 |
| Total |
248 |
4.2 | 192 | 4.2 |
0.9266 |
All cells less than 10 were marked as “<10” and their corresponding percentages were not reported (NR).
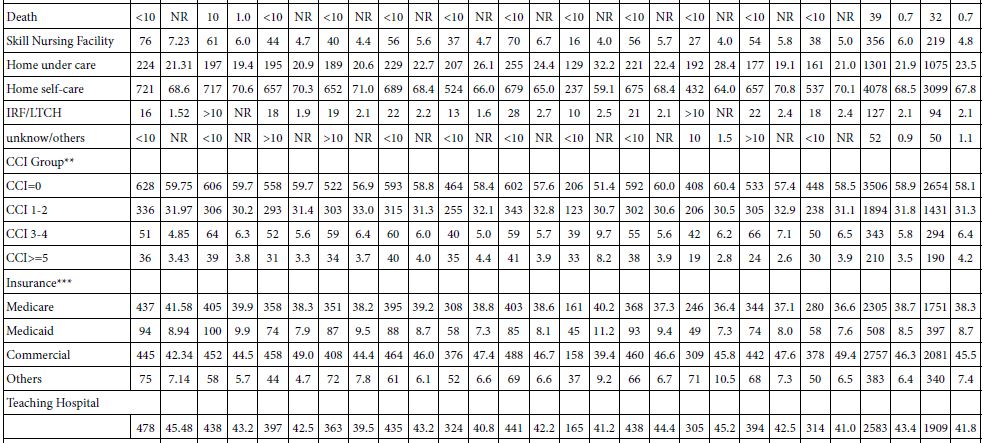
Adverse Events
There was no difference in the rates of the majority of postoperative complications including superficial surgical site infection, gastrointestinal bleeding, hemorrhage, or urinary tract infection. However, other postoperative complications such as sepsis were significantly higher (6.8%) in April 2020 as compared to the same time period 1 year earlier (3.4%; p<0.005) (Table 5). Similarly, there were statistically significant increases in the rates of postoperative peritonitis or organ space infection as well as ileus/small bowel obstruction in the month of April 2020 compared to April 2019. However, when controlling for the urgent nature of the operation, the rate of all postoperative complications including sepsis became statistically equivalent between the 2019 and 2020 time periods except for organ space infection (OR=1.20 95% CI:1.10-1.31; p<0.001).
Table 5: Post-operative adverse events.
| 2019 | 2020 | |||||
| N | % | N | % |
p-value |
||
| Ileus/ Small Bowel Obstruction (included constipation and PONV) | ||||||
| Jan | 161 | 15.4 | 149 | 14.6 | 0.6843 | |
| Feb | 126 | 13.4 | 125 | 13.6 |
0.9368 |
|
| Mar | 132 | 13.0 | 113 | 14.2 |
0.4847 |
|
| Apr | 146 | 14.0 | 75 | 18.8 |
0.0252 |
|
| May | 134 | 13.6 | 119 | 17.6 | 0.0239 | |
| Jun | 133 | 14.4 | 109 | 14.2 |
0.9523 |
|
|
Total |
832 | 14.0 | 690 | 15.1 |
0.1037 |
|
| Peritonitis/Organ space SSI | ||||||
|
Jan |
234 | 22.2 | 264 | 26.0 | 0.0466 | |
| Feb | 196 | 21.0 | 262 | 28.6 |
0.0002 |
|
|
Mar |
272 | 27.0 | 231 | 29.0 | 0.3217 | |
| Apr | 260 | 24.8 | 131 | 32.6 |
0.0028 |
|
|
May |
271 | 27.4 | 211 | 31.2 | 0.0934 | |
| Jun | 231 | 24.8 | 205 | 26.0 |
0.3809 |
|
|
Total |
1464 | 24.6 | 1304 | 28.5 |
<0.0001 |
|
| Superficial SSI and wound complications (Hematoma/ Seroma, Wound Infection, Wound Dehiscence) | ||||||
|
Jan |
26 | 2.4 | 19 | 1.8 | 0.3488 | |
| Feb | 22 | 2.4 | 21 | 2.2 |
0.9227 |
|
|
Mar |
22 | 2.2 | 19 | 2.4 | 0.7662 | |
| Apr | 31 | 3.0 | 16 | 4.0 |
0.3258 |
|
|
May |
23 | 2.4 | 20 | 3.0 | 0.4249 | |
| Jun | 14 | 1.6 | 15 | 2.0 |
0.4777 |
|
|
Total |
138 | 2.3 | 110 | 2.4 |
0.7645 |
|
| GI bleeding | ||||||
|
Jan |
66 | 6.2 | 63 | 6.2 | 0.9455 | |
| Feb | 54 | 5.8 | 48 | 5.2 |
0.6021 |
|
|
Mar |
59 | 5.8 | 47 | 6.0 | 0.9527 | |
| Apr | 58 | 5.6 | 24 | 6.0 |
0.7489 |
|
|
May |
54 | 5.4 | 48 | 7.2 | 0.1713 | |
| Jun | 50 | 5.4 | 42 | 5.4 |
0.9315 |
|
|
Total |
341 | 5.7 | 272 | 6.0 |
0.6253 |
|
| Urinary tract infection/Retention of urine | ||||||
|
Jan |
90 | 8.6 | 63 | 6.2 | 0.0409 | |
| Feb | 61 | 6.6 | 54 | 5.8 |
0.563 |
|
|
Mar |
63 | 6.2 | 49 | 6.2 | 0.9452 | |
| Apr | 70 | 6.6 | 38 | 9.4 |
0.0721 |
|
|
May |
62 | 6.2 | 42 | 6.2 | 0.9608 | |
| Jun | 55 | 6.0 | 52 | 6.8 |
0.468 |
|
|
Total |
401 | 6.7 | 298 | 6.5 |
0.6624 |
|
| MI/Cardio complication | ||||||
|
Jan |
46 | 4.4 | 53 | 5.2 | 0.3687 | |
| Feb | 40 | 4.2 | 45 | 5.0 |
0.5243 |
|
|
Mar |
51 | 5.0 | 38 | 4.8 | 0.7901 | |
| Apr | 45 | 4.4 | 31 | 7.8 |
0.009 |
|
|
May |
65 | 6.6 | 35 | 5.2 | 0.2384 | |
| Jun | 33 | 3.6 | 43 | 5.6 |
0.0417 |
|
|
Total |
280 | 4.7 | 245 | 5.4 |
0.124 |
|
| Sepsis | ||||||
|
Jan |
25 | 2.4 | 37 | 3.6 | 0.0916 | |
| Feb | 30 | 3.2 | 24 | 2.6 |
0.4447 |
|
|
Mar |
31 | 3.0 | 32 | 4.0 | 0.2733 | |
| Apr | 35 | 3.4 | 27 | 6.8 |
0.0045 |
|
|
May |
23 | 2.4 | 14 | 2.0 | 0.7281 | |
| Jun | 35 | 3.8 | 21 | 2.8 |
0.2379 |
|
|
Total |
179 | 3.0 | 155 | 3.4 |
0.2635 |
|
| Dehydration/ Acute renal failure | ||||||
|
Jan |
131 | 12.4 | 127 | 12.6 | 0.9737 | |
| Feb | 111 | 11.8 | 104 | 11.4 |
0.7091 |
|
|
Mar |
123 | 12.2 | 108 | 13.6 | 0.3776 | |
| Apr | 122 | 11.6 | 60 | 15.0 |
0.0915 |
|
|
May |
105 | 10.6 | 96 | 14.2 | 0.0278 | |
| Jun | 102 | 11.0 | 79 | 10.4 |
0.653 |
|
|
Total |
694 | 11.7 | 574 | 12.6 |
0.1576 |
|
| Hemorrhage | ||||||
|
Jan |
41 | 4.0 | 38 | 3.8 | 0.8522 | |
| Feb | 39 | 4.2 | 42 | 4.6 |
0.6742 |
|
|
Mar |
36 | 3.6 | 33 | 4.2 | 0.5208 | |
| Apr | 45 | 4.4 | 15 | 3.8 |
0.6293 |
|
|
May |
29 | 3.0 | 29 | 4.2 | 0.1384 | |
| Jun | 29 | 3.2 | 33 | 4.4 |
0.1968 |
|
|
Total |
219 | 3.7 | 190 | 4.2 |
0.2071 |
|
Mortality
In hospital mortality occurred rarely in patients treated for diverticulitis. The proportion of patients who experienced an inpatient mortality was 0.7% in both time periods (Table 1).
Discussion
Data from these analyses reveal a substantial decline in the number of inpatients with diverticulitis during the height of the COVID-19 pandemic or the first two quarters of 2020 as compared to the same time period in 2019. Despite the net decline in diverticulitis admissions, the proportion of cases deemed urgent rose significantly during COVID-19. In addition, there was a marked reduction in the proportion of patients who had minimally invasive surgery during the COVID surge in early 2020. These changes were associated with a temporal increase in sepsis and deep organ space complications in April of 2020. However, this observed increase in postoperative complications during the COVID-19 period became statistically insignificant when accounting for the emergent nature of the operations, with the exception of organ space infection likely secondary to the higher rate of preoperative abscesses. Of great importance, despite high numbers of COVID-19 hospitalizations during the height of the pandemic, there was no increase in respiratory complications. These results indicate that surgery for diverticulitis (both urgent and elective) can be safely performed without any additional increase in respiratory consequences or mortality.
Across the board, many patients with non-respiratory health conditions delayed or avoided care during the height of the COVID-19 pandemic. A number of studies demonstrated reduced emergency room visits across the United States and United Kingdom during the height of the COVID-19 pandemic, including fewer evaluations for acute coronary syndromes and strokes [9-17]. Similarly, our data confirm fewer admissions for diverticular disease as total numbers declined by 25 percent during the height of the pandemic. In addition, among the patients who were admitted for diverticular disease, proportionately more patients were admitted with much more severe disease (i.e. abscess) leading to far greater rates of stoma creation as compared to one year prior.
There are a number of possible explanations for the decline in numbers of diverticulitis admissions during the height of the COVID-19 pandemic. Although lifestyle changes during this time may be one explanation, it is more likely that many patients simply deferred evaluation because of anxiety related to management during the pandemic. In a survey of adult respondents, 40.9% reported having delayed or avoided any medical care, including urgent or emergency care (12.0%) and routine care (31.5%), because of concerns about COVID-19 [18]. Avoidance of routine care was particularly common among unpaid caregivers who sought to avoid potential virus risk for many reasons. Data do reveal that it is difficult for patients to anticipate when emergency department evaluation is necessary [19]. As with other studies our data similarly raise concerns about patients deferring care and presenting to the emergency department when diverticulitis progressed to more complicated forms [20].
In addition to patient avoidance of routine care, many healthcare services underwent paradigm shifts in order to more safely deliver care while reducing potential points of transmission. Elective procedures were prohibited leading to sharp declines across the board for many orthopedic conditions as we also noted with diverticular disease. Delays in surgery are likely to have real impact on patient health outcomes, hospital finances and resources, as well as training and research programs [21]. Delays in surgery have been shown to result in higher rates of surgical site infections, leading to increased costs ranging from $7000 to $17,000 for coronary artery bypass graft and colon and lung resections [22]. It is unclear what the costs of delay in care may be for patients with diverticulitis, but an increase in septic complications was noted during the height of the COVID-19 pandemic.
To promote safe surgery many surgical societies as well as Intercollegiate guidelines from the United Kingdom advocated for non-operative management of many surgical conditions and avoidance of laparoscopy when surgery is unavoidable [23]. The effects of these guidelines on appendicitis treatment in the United Kingdom was associated with many practice changes during the pandemic [20]. Early concerns were also raised involving the risk of aerosolization with minimally invasive surgery in the operating room. Many hospitals began to screen patients for the virus before any scheduled surgery and when not possible, personal protective equipment to decrease susceptibility to aerosol diffusion was advised. As expected, we identified a reduction in the rate of laparoscopic treatment during the pandemic which may have been related to the suggested guidelines. It is, however, highly likely that the changes we noted in use of laparoscopy may have been related to more severe diverticular disease.
Interestingly, in the previously described appendicitis study (English et al.), the investigators did not notice an increase in short-term complications nor any detriment in length of stay related to appendicitis treatment during COVID [20]. Our data, however, revealed a significant change in septic complications during the height of the COVID-19 pandemic following surgery for diverticular disease. In addition, there were substantial concerns of pulmonary complications related to surgical treatment. Our data from 586 hospitals across the country indicate no significant increase in pulmonary complications throughout the study period, with only slight increase during the single month of April. After accounting for disease severity, this difference became insignificant.
Conclusions
In conclusion, data from these studies reveal deferral of care in patients with diverticular disease during the COVID-19 pandemic. Patients who did seek care for diverticulitis experienced no additional respiratory complications. Given that postoperative pulmonary complications occur in half of patients with perioperative COVID-19 infection, regardless of whether the diagnosis is made with laboratory-confirmation or due to clinical signs, these data can be used to reassure patients needing surgery [24]. Some have advocated that during COVID-19 outbreaks, consideration should be given for postponing non-critical procedures [25]. However, as we prepare for future waves of COVID cases, these studies may help us answer questions related to patient safety while reassuring our patients regarding surgical care. Awareness of community COVID-19 prevalence, testing, as well as patient and provider preparedness are critical elements of surgical care during respiratory pandemics.
References
- Cucinotta D, Vanelli M (2020) WHO Declares COVID-19 a Pandemic. Acta Biomed 91: 157-160. [crossref]
- WHO Director-General’s opening remarks at the media briefing on COVID19 – March 2020.
- Healthcare Facilities: Managing Operations During the COVID-19 Pandemic. National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases.
- Schrag D, Hershman DL, Basch E (2020) Oncology practice during the COVID-19 pandemic. JAMA 323: 2005-2006. [crossref]
- van de Haar J, Hoes LR, Coles CE, Seamon K, Frohling S, et al. (2020) Caring for patients with cancer in the COVID-19 era. Nat Med 26: 665-671. [crossref]
- Sharpless N (2020) COVID-19 and cancer. Science 368: 1290.
- Premier Data. Available at https://products.premierinc.com/downloads/PremierHealthcareDatabaseWhitepaper.pdf
- Charlson M, Wells MT, Ullman R, King F, Shmukler C (2014) The Charlson comorbidity index can be used prospectively to identify patients who will incur high future costs. PloS One 9: e112479. [crossref]
- Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG (2020) Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. Journal of Stroke and Cerebrovascular Diseases 29: 104953.
- Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, et al. (2020) Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 75: 2871-2872. [crossref]
- Bullrich MB, Fridman S, Mandzia JL, Mai LM, Khaw A, et al. (2020) COVID-19: Stroke Admissions, Emergency Department Visits, and Prevention Clinic Referrals. Canadian Journal of Neurological Sciences 47: 693-696. [crossref]
- Morelli N, Rota E, Terracciano C, Immovilli P, Spallazzi M, et al. (2020) The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol 83: 213-215. [crossref]
- Kansagra AP, Goyal MS, Hamilton S, Albers GW (2020) Collateral effect of Covid-19 on stroke evaluation in the United States. New England Journal of Medicine 383: 400-401. [crossref]
- Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, et al. (2020) The Covid-19 pandemic and the incidence of acute myocardial infarction. New England Journal of Medicine 383: 691-693. [crossref]
- Kim HS, Cruz DS, Conrardy MJ, Gandhi KR, Seltzer JA, et al. (2020) Emergency department visits for serious diagnoses during the COVID-19 pandemic. Acad Emerg Med 27: 910-913. [crossref]
- Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD (2020) An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med 76: 595-601. [crossref]
- Jeffery MM, D’Onofrio G, Paek H, Platts-Mills TF, Soares WE, et al. (2020) Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med 180: 1328-1333. [crossref]
- Czeisler MÉ, Marynak K, Clarke KE, Salah Z, Shakya I, et al. (2020) Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns–United States, June 2020. MMWR Morb Mortal Wkly Rep 69: 1250-1257.
- Coster JE, Turner JK, Bradbury D, Cantrell A (2017) Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med 24: 1137-1149. [crossref]
- English W, Bedwani NB, Smith C, Doganay E, Marsden M, et al. (2020) Suspected appendicitis and COVID-19, a change in investigation and management-a multicentre cohort study. Langenbecks Arch Surg 406: 357-365. [crossref]
- Fu SJ, George EL, Maggio PM, Hawn M, Nazerali R (2020) The Consequences of Delaying Elective Surgery: Surgical Perspective. Ann Surg 272: e79-e80. [crossref]
- Vogel TR, Dombrovskiy VY, Lowry SF (2010) In-hospital delay of elective surgery for high volume procedures: the impact on infectious complications. J Am Coll Surg 211: 784-790. [crossref]
- Mowbray NG, Ansell J, Horwood J, Cornish J, Rizkallah P, et al. (2020) Safe management of surgical smoke in the age of COVID-19. Br J Surg 107: 1406-1413. [crossref]
- COVID Surg Collaborative (2020) Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 396: 27-38.
- American College of Surgeons. COVID-19: guidance for triage of non-emergent surgical procedures. https://www.facs.org/covid-19/clinical-guidance/triage. Date: March 17, 2020.