DOI: 10.31038/CST.2018313
Abstract
In children and adolescents, primary osteosarcoma is one of the most common malignant bone tumors. It principally affects the long bones, especially in the distal femur, proximal tibia and proximal humerus. Osteosarcoma rarely arises from flat bone, and as in this patient’s case, osteosarcoma of the rib is very infrequent. To the best of our knowledge, this is the first reported case of rib osteosarcoma in our country. Here we report a case of conventional rib osteosarcoma presenting as chest pain and mass that successfully had complete pathologic response with clear margins after four cycles of neoadjuvant therapy.
Introduction
Osteosarcomas principally originate in the metaphysis of the long bones. Approximately 10% of osteosarcomas originate in the flat bones, with the pelvis being the main site. Roughly 1 – 2% of osteosarcoma occur in the thoracic bones inclusive of the ribs, sternum, and clavicle [1]. The prevalence of osteosarcoma is in the second decade of life with another spike in older individuals after radiation or Paget’s disease [2]. Osteosarcoma of the rib have been reported in older children ranging from 7 to 13 years of age [3]. Diagnosis of osteosarcoma of the rib is a challenge for most physicians since the commonest presentation is pain and a palpable chest wall mass. The lesion is usually observed on a chest radiograph as a soft tissue mass. Limiting factors for its diagnosis is the difficulty visualizing typical periosteal reaction, rib destruction and calcifications within the mass in a chest radiograph compared to the site of the tumour if it were in a long bone. We present rare location of an osteosarcoma which posed a diagnostic challenge to both the pathologist and the physician in a young male.
Case Report
This is a case of an 18 year old Filipino male, apparently well until two months before consult, noted intermittent right upper quadrant pain. He later palpated a pea sized firm, movable, non-tender mass at the right upper quadrant area. Neither medications nor consult done until two months later noted gradual progression of the mass. It was approximately 3 x 3 cm in size with intermittent pain and occasional dyspnea. Consult done to a local hospital where chest radiograph was done revealing right pleural effusion. Underwent chest thoracostomy tube insertion was cytology negative for malignancy. Chest Computed tomography (Figure 1) done June 2016 revealed lobulated heterogenously enhancing mass lesion in antero-inferior aspect of right hemithorax measuring 5.3x 5.4 x 5.01 cm. Right paratracheal subcentimeter lymph nodes. Abdominal CT scan was unremarkable. Patient underwent excision biopsy of the mass at eighth rib revealed conventional osteosarcoma, osteoblastic type high grade
(Figures 2 and 3). Tumor size of 3.5 cm, no definite vascular invasion with tumor invasion into extra-osseous soft tissues and present in inked tissue edges. Diaphragmatic tumor was also noted to be high grade osteosarcoma.
Figure 1. lobulated heterogeneously-enhancing mass lesion in the antero-inferior aspect of the right hemithorax measuring 5.3 × 5.4 × 5.01 cm in cranio-caudad, transverse and antero-posterior diameters. Mass cannot be separated from the expanded and lytic change anterior aspect of the right 8th rib with associated overlying soft tissue swelling and indentation into the superior-anterior margin of right hepatic lobe
Figure 2. Low power field magnification
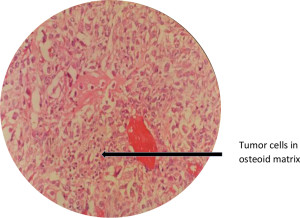
Figure 3. High power field magnification several highly atypical spindle cells producing tumor osteoid. The cells have enlarged, hyperchromatic nuclei with prominent nucleoli. Brisk mitotic activity is seen.
He was referred to a Medical Oncologist where he underwent four sessions of neoadjauvant chemotherapy from June 23-August 29, 2016 with Doxorubucin (25mg/m2) and Cisplatin (50mg/m2) days 1-3 every 21 days. He tolerated the therapy well, no adverse events. Re-evaluation scans done September 27, 2016 showed Interval resolution of right sided pleural effusion. Right 7th anterior rib is surgically absent with stable post interventional change in right serratus anterior muscle. He was then referred to Thoracic Surgeon for surgery. Pre-operative pulmonary function test was unremarkable. He underwent video-assisted thoracic surgery, right converted to thoracostomy with chest wall reconstruction using bone cement for four hours and 26 minutes. Post-operative findings were dense pleural adhesions from apex down to diaphragm, no gross tumor noted along chest wall, diaphragm and pleura. Resection extended one rib above and one rib below (6th and 8th ribs). Specimen was sent to histopathology laboratory with later findings of fibrosis, haemorrhage and negative for tumor of pleural nodule and right lateral chest wall (Figures 4, 5 & 6). No residual tumor and negative lines of resection for the 6th and 8th ribs.
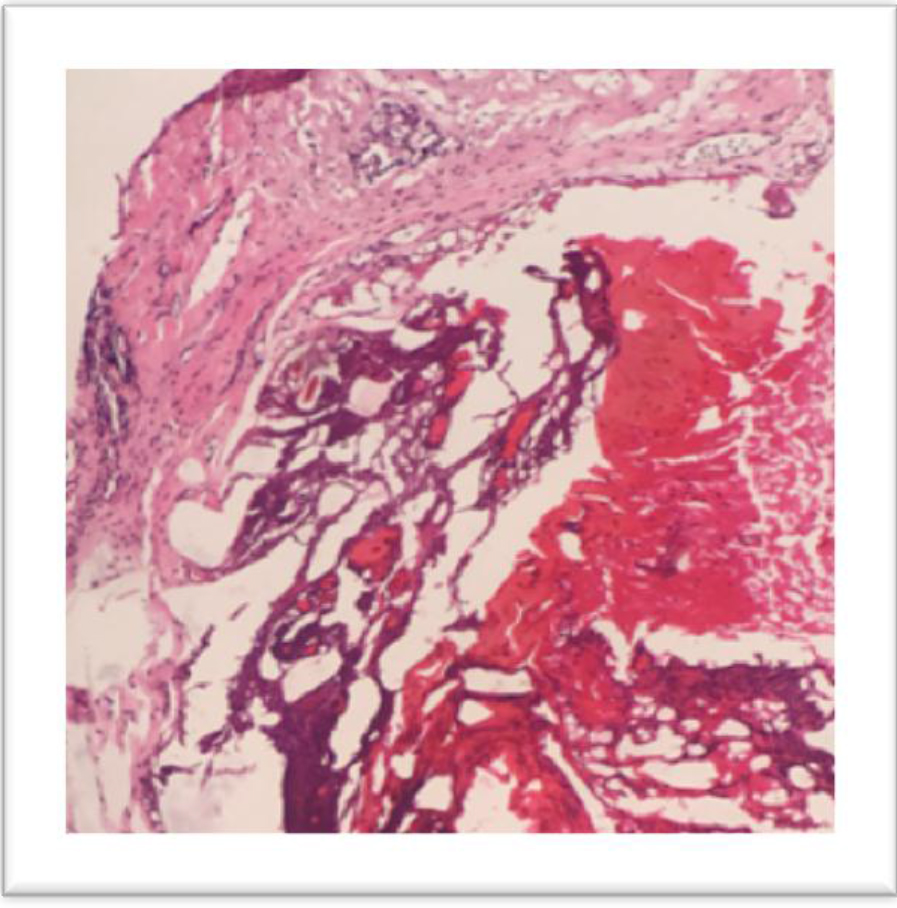
Figure 4. Pleural Nodule, Right, Lateral Chest Wall, Diaphragm: Fibrosis, Old haemorrhage. No tumor present
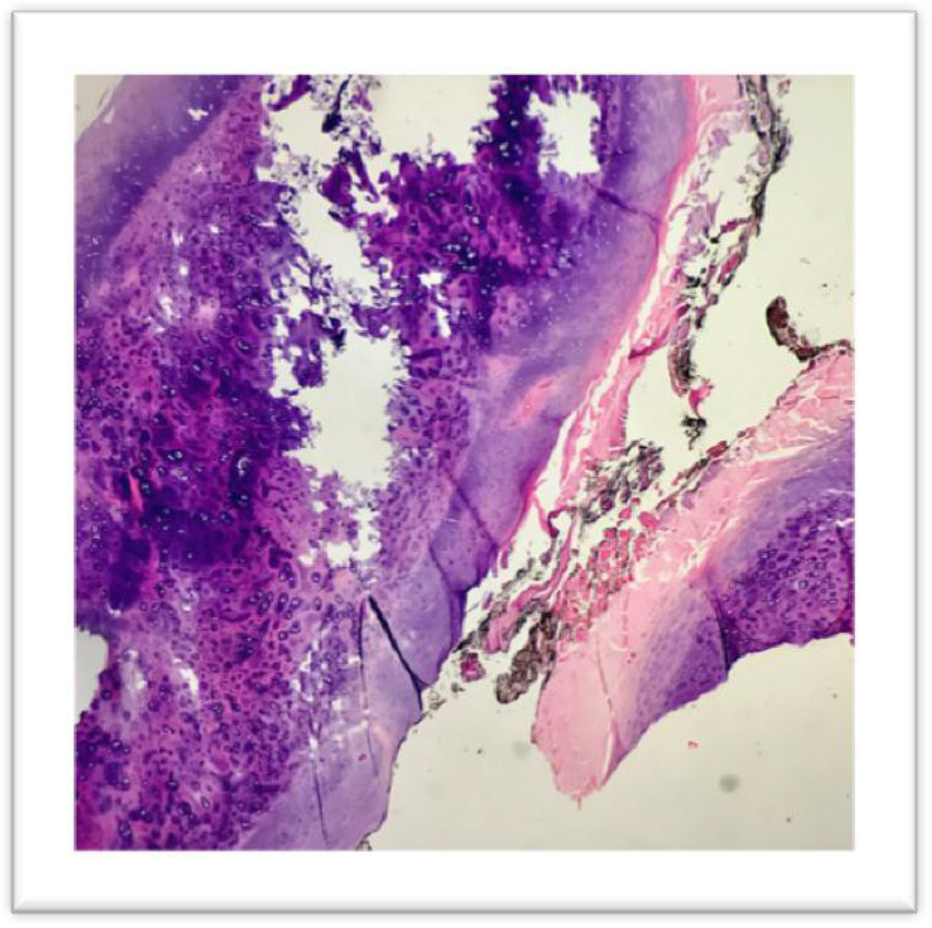
Figure 5. Ribs 6-8th, chest wall resection: No residual tumor, fibrosis, granulation tissue
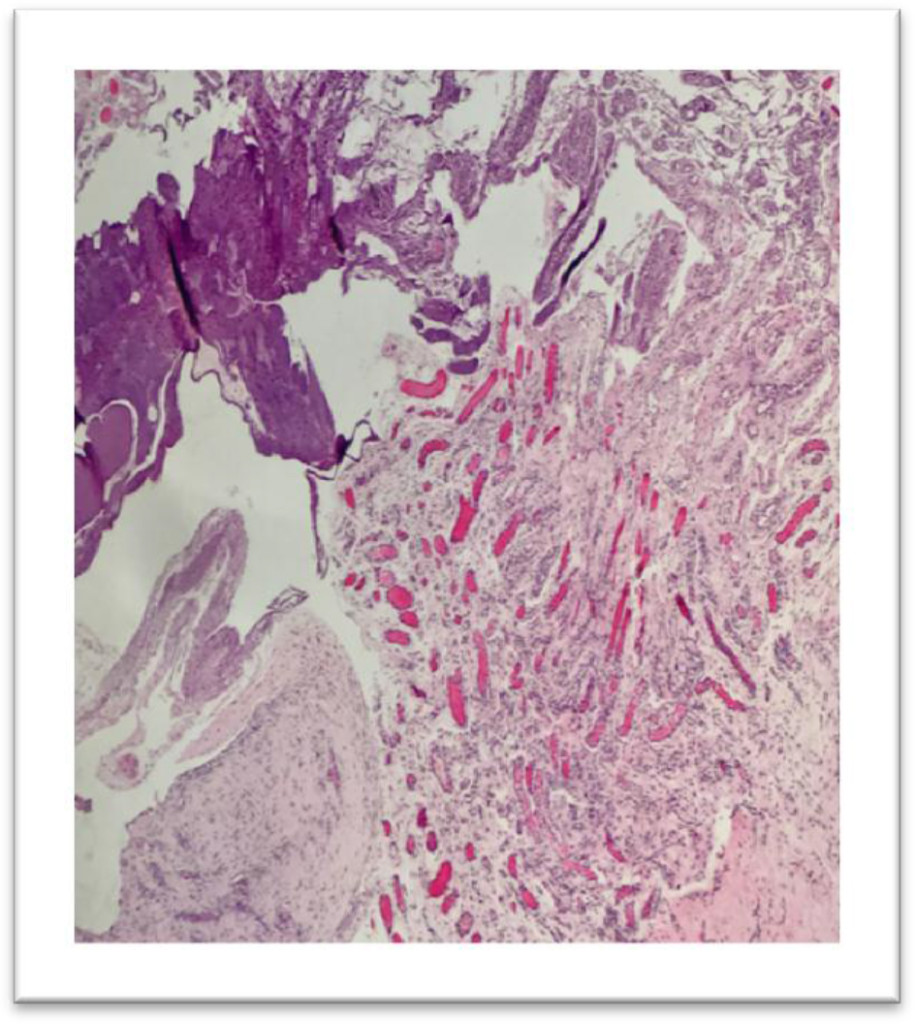
Figure 6. Pleural Nodule, Diaphragm, Right, Parietal Pleura: fibrosis and granulation tissue formation. Negative for tumor
Surveillance studies done on the 3rd, 6th and 9th month post-surgery were unremarkable. Chest CT scan (Figure 7) done did not show discrete enhancing mass in the anterolateral chest wall to suggest tumor recurrence and enlarged lymph nodes. Latest CT scan done July 21, 2017. Patient is back to school with no symptoms.

Figure 7. Surveillance chest CT scan: The RIGHT antero-lateral 6th to 8th ribs are surgically absent. No pulmonary mass or nodule.
Discussion
Chest computerized tomography examination is useful for identification and characterisation of the mass. Invasion to deeper structures like the muscles, pleura and lungs can also be accurately assessed with the aid of a CT scan as compared to plain radiograph. CT would be a more cost effective modality for evaluating the tumour since a magnetic resonance imaging (MRI) may not offer any additional information.3 Therefore, accurate diagnosis is an essential component in survival of these patients. Histopathological diagnosis is imperative in instituting a definite therapy. The classic feature of a ramifying osteoid matrix laid down by the neoplastic cells clinches the diagnosis and enables one to exclude all the other possible differentials.
Conventional osteosarcomas are the most aggressive osseous neoplasms. The overall prognosis of osteosarcoma in flat bones remains poor because of the difficulty of complete excision. The guidelines for management and the prognosis and survival rates in rib primary OS is not clear due to the small number of cases studied. However, there is documentation of better survival in patients who have had a complete resection of their tumor at the time of surgery [4]. A local wide excision with removal of the involved ribs and subsequent reconstruction using a mesh followed by adjuvant chemotherapy and radiotherapy may improve survival in these patients. Although osteosarcoma of flat bones is rarely associated with metastasis, it is still advised to include a CT scan of the thorax, chest x-rays, and bone scans as part of the diagnostic tool in order to look for metastasis.
The treatment of osteosarcoma generally consists of local excision with a wide margin [5]. It still remains to be unresolved exactly what size of margin is optimal. Palliative chemotherapy or radiotherapy may also be considered for those who undergo a palliative surgery since >80% of patients, local recurrence appears in the absence of a wide resection.
Conclusion
This case highlights the importance of including the diagnosis of osteosarcoma, although rare, as a differential diagnosis of primary malignant neoplasm of the rib. Point tenderness in the young also warrants further investigation for it may just be the sole manifestation of a treatable case as morbid as malignancy.
References
- Mirra JM, Gold RH, Picci P (1989) Osseous tumors of intramedullary origin. In: Mirra JM, editor. Bone Tumors: Clinical, Radiological, and Pathological Correlations. Philadelphia: Lea and Febiger; 143–438.
- Burt M, Fulton M, Wessner-Dunlap S, Karpeh M, Huvos AG, et al. (1992) Primary bony and cartilaginous sarcomas of chest wall: results of therapy. Ann Thorac Surg 54: 226–232. [crossref]
- Deitch J, Crawford AH, Choudhury S (2003) Osteogenic sarcoma of the rib: a case presentation and literature review. Spine (Phila Pa 1976) 28: E74–77. [crossref]
- Xu, J. and Yao, Q. and Hou, Y. and Xu, M. and Liu, S. and Yang, L. and Zhang, L. and Xu, H (2013) MiR-223/Ect2/p21 signaling regulates osteosarcoma cell cycle progression and proliferation. Biomedicine and Pharmacotherapy. 67: 381–386
- Funovics PT, Bucher F, Toma CD, Kotz RI, Dominkus M (2011) Treatment and outcome of parosteal osteosarcoma: biological versus endoprosthetic reconstruction. J Surg Oncol 103:782–9.