DOI: 10.31038/CST.2018322
Abstract
Introduction: The paper presents the assessment of radiation doses received by patients undergoing mammography imaging at Mulago National Referral and Teaching Hospital for a period of five months.
Materials and Methods: Mammography polymethyl methacrylate (PMMA) phantoms of different sizes were used in the determination of the doses to the breast of patients. Mean glandular doses (MGDs) of 60 patients who presented for mammography within the study period were determined from their exposure data, the tube output, and half-value layer (HVL) of the mammography unit. The kVp, mAs, compressed breast thickness (CBT), and projection view (Mediolateral oblique projection, MLO /Cranial-caudal projection, CC) for each patient were then used to expose the phantoms simulating the different patients’ CBT. The MGD was calculated as the product of the entrance surface dose (ESD) at the surface of the phantom and the conversion factors extracted from the European protocol on dosimetry in mammography, EUR 16263, 1996. Thermoluminescent dosimeters (TLDs) were used in the measurement of the ESD.
Results: The average MGD was 1.6 ± 0.5 (range 0.8 – 2.5) mGy for CC projection and 1.7 ± 0.3 (range 1.1 – 2.4) mGy for the MLO projection. The MGD for a 4.5 cm CBT was 1.6 ± 0.1 mGy and 1.8 ± 0.01 mGy for CC and MLO projections respectively which were both less than 3.0 mGy recommended by the American College of Radiology.
Conclusion: The values of MGD found in this study were therefore acceptable and comparable to the recommended standards by the American College of Radiology.
Key words
mammography, mean glandular dose, phantom, thermoluminescent dosimeter.
Introduction
Breast cancer cases are rising worldwide especially across the developing world [1]. Women breast cancer is the main cause of cancer mortality in women globally. In Uganda, it comes third after cervical cancer and Kaposi’s sarcoma [2]. Presently, breast cancer has no effective primary prevention. Early detection of breast cancer can help treat and cure the disease. International Atomic Energy Agency (IAEA) report on radiation protection of patients shows that mammography is very good at early identification and diagnosing of breast cancer and has decreased mortality mostly in women of age 50-69 years to up to 20% – 35% reductions (IAEA-RPOP, 2014). It therefore implies that efforts need to be made to detect breast cancer while still in its early and treatable stages [2].
Mammography helps in identifying very small breast tumors with the aim of detecting breast cancer when it is still in its treatable conditions. Mammography necessitates control over management of patient dose and reduction of possible risk since the breast glandular tissue is very sensitive to ionizing radiation [3]. Mammography calls for use of X-rays that have the potential to cause cancer, but the advantages of mammography weigh more than any possible harm that may result from radiation exposure [4]. A balance between image information and the absorbed dose to the patient’s breast always needs to be taken into account i.e. the dose should be kept as low as reasonably achievable [5].
The radiation exposure of a mammography patient is expressed in terms of the mean glandular dose (MGD). The MGD is the mean dose to the breast glandular tissue. It is taken to be an important quantity for establishing risk from different mammography procedures [6]. However, the MGD cannot be measured directly as it occurs within the breast. MGD for each patient is got from calculations involving exposure parameters used to obtain the mammogram and the measurement of tube output [6]. It is very essential that the dose experienced by patients as a result of exposure to radiation is optimum, therefore the MGD is pertinent ( Elsie et al., 2010) to Mammography. The American College of Radiology, 2014 recommendation on MGD for a 4.5 cm compressed breast thickness is less than 3 mGy for screen/film with grid.
This study aims at determining and assessing the radiation doses received by patients undergoing mammography imaging at Mulago National Referral and Teaching Hospital.
Materials and Methods
Study Design
The performance of the mammography machine was tested by investigating the accuracy and reproducibility of the kVp settings and measuring the half value layer (HVL).
Patients’ consent was sought and their data and exposure parameters used for mammography examination were recorded by the Mammographer on the exposure data form. The exposure parameters recorded included the patient’s age, Tube potential (kVp), Tube loading (mAs), compressed breast thickness (CBT), projection view, and whether the right or left breast was exposed. Since radiation exposure of humans for medical research is deemed to be unjustified [7] mammography polymethyl methacrylate (PMMA) phantoms of different sizes were used to simulate the different patient breast sizes. The PMMA phantoms were exposed using the same exposure parameters as were used on different patients to obtain the entrance surface dose (ESD) that was received by each patient in each projection view.
Calculations were then done to determine the mean glandular doses (MGDs) that were received by the patients.
Materials
The equipment and tools used for collecting data consisted of the mammography machine, a digital kVp meter (Unfors Mult-O-Meter) type 535L, PMMA mammography phantoms that were used to evaluate radiation dose and were tested to ensure that they simulated radiographic features of the breast tissue, Thermoluminescent dosimeters (TLD badges) that were used in measurement of entrance surface dose (ESD). Lithium Fluoride TLD 100 (LiF TLD-100) badges with two chips were used and the average reading of both chips was taken [8].
The TLD badges were calibrated using caesium 137 Irradiator, and annealed before they were exposed to radiation. The TLD badges were read from the laboratory of the Physics Department of Makerere University using the Harshaw 4500 TLD reader, which was calibrated using the Strontium-90 (Sr-90) Irradiator (model 2000) [9].
The Mammography Machine
The mammography machine used was a Philips Mammo Diagnost UC with serial number 885538968. Its focal spot size was 0.3 mm and it used a high frequency X-ray generator. The machine’s exposure voltage ranged from 23 to 35 kV, adjustable in increments of 1 kV. The filter used was molybdenum (Mo) and the target/filter combination was Mo/Mo. The compressed breast thickness (CBT) was measured by an inbuilt device (ruler) whose accuracy was verified. Calibration and full quality control measurements were also made on the machine according to the requirements of the regulatory authority. Preliminary tests were done on the machine to ensure proper function for example testing for accuracy and reproducibility of kVp settings, and measurement of half value layer (HVL). The instrument used for these measurements was the Unfors Mult-O-Meter (Model 535L, Serial Number 147389), which was used for both half value measurements (as a dosimeter) and for kVp measurements. The Unfors Mult-O-Meter was calibrated using a Siemens Mammomat 3000 with a Mo anode and 30 µm Mo added filtration [10].
Determining Radiation Doses Received by Patients
Doses of 60 patients who presented for mammography within a period of five months were calculated from patient exposure data and from the measurements of tube output and HVL of the mammography unit. For every mammogram obtained, an assessment for image quality compliance was carried out by qualified radiologists. The MGD was determined for different patients using polymethyl methacrylate (PMMA) phantoms of different sizes, imaged using the same parameters as were used on patients. The tube output was determined as the ratio of entrance surface dose (ESD) and mAs at a distance of 0.6 m. I.e.
TLDs were used in the measurement of ESD. In measurement of ESD, the mammography machine was set up for either cranial-caudal (CC) or mediolateral oblique (MLO) projection view with the compression plate present. The MLO projection was performed at 45o. For each patient’s breast thickness, a representative phantom was positioned on the breast support and a TLD placed on top of the phantom (at the reference point). An exposure was made using the same parameters as used clinically on patients. The TLDs were then kept away from radiation and later taken to the laboratory for reading [11-13].
The MGDs were calculated according to the European protocol on dosimetry in mammography, 1996 as;
MGD = KPMMA × g × c
Where KPMMA is the incident air kerma at the surface of the phantom, (KPMMA = Tube output × Tube loading, mAs), g-factors convert air kerma into dose, c-factors correct for different glandularity than 50%, and both g- and c-factors depend on the HVL and CBT. The HVL was determined and found to be 0.42 mm.
The distribution of MGDs for both CC and MLO views for the different breast sizes was determined.
Results
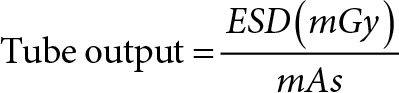
The distribution of entrance surface dose (ESD) of both CC and MLO views for the different tube potentials were as shown in Table 1, and represented in a histogram in Figure 1.
Figure 1. Distribution of ESD for different tube potentials (kVp) for both CC and MLO views.
Table 1. ESD for the different tube potentials for both CC and MLO views
|
ESD ± 0.01(mGy) |
||
|
Tube Potential (kVp) |
CC |
MLO |
|
22 |
3.76 |
3.85 |
|
23 |
4.96 |
4.64 |
|
24 |
5.90 |
5.28 |
|
25 |
7.29 |
6.95 |
|
26 |
8.94 |
7.93 |
|
27 |
10.11 |
9.53 |
|
28 |
11.24 |
10.16 |
|
29 |
13.41 |
12.05 |
Table 2 shows the kVp values that were used for the different CBT. The CBT was measured as the distance between the bottom of the compression plate and the table upon which the breast rested. This was done using an in built device (ruler) whose accuracy was verified.
Table 2. kVp range used for the various CBT
|
CBT (cm) |
2.5 |
3.0 |
3.5 |
4.0 |
4.5 |
5.0 |
5.5 |
6.0 |
6.5 |
7.0 |
|
kVp used |
22-25 |
22-25 |
22-26 |
22-28 |
23-26 |
22-28 |
25-29 |
25-26 |
26-28 |
27-29 |
The MGD per projection view for each patient was determined by multiplying the ESD by the conversion factors which are a function of half value layer (HVL) and compressed breast thickness (CBT). The conversion factors used in this study were those by Dance et al, extracted from the European protocol on dosimetry in mammography, 1996. The average value of MGD per CBT for the two projection views was determined and plotted as shown in Figure 2 below.
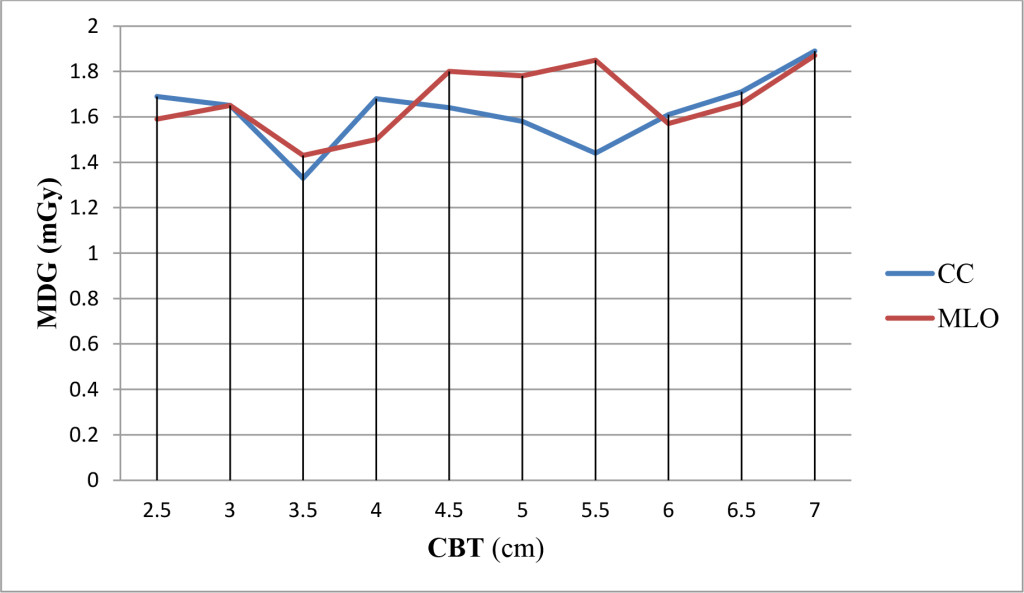
Figure 2. Average of MGD for the different CBT for the two projection views.
The average MGD was 1.6 ± 0.5 (range 0.8 – 2.5) mGy for the CC projection and 1.7 ± 0.3 (range 1.1 – 2.4) mGy for the MLO projection. The average MGD for a 4.5 cm CBT was found to be 1.6 ± 0.1 mGy and 1.8 ± 0.01 mGy for the CC and MLO projections respectively.
Discussion
From figure 1 above, the values of ESD for CC view for a given kVp value were found to be generally higher than those for MLO view. This is because with MLO view, more breast tissue is imaged thereby providing extra tissue without extra exposure, hence lower values of ESD.
There was some non uniformity in the distribution of kVp values for the various CBT. E.g. Patients with 2.5 cm, 3.0 cm and 3.5 cm CBT were exposed using almost the same kVp range, some patients of 5.0 cm CBT were exposed using kVp as low as 22 kVp. This implies therefore that some patients with lower CBT could be found to have received higher MGD as compared to some with higher CBT. This was however a result of difference in patient breast density.
There was a fluctuation in the distribution of MGD for the different CBT (Figure 2). This was due to the difference in kVp used for the different CBT. The average dose values obtained of 1.6 ± 0.5 mGy for CC projection and 1.7 ± 0.3 mGy for MLO projection view were found to be less than those found in the study done in Kenya by JS Wambani et al; 2011, where the average MGD was 2.14 and 2.44 mGy for CC and MLO projection views respectively and also less than those obtained in a study done in Bulgaria by Simona and Jenia; 2008, on two mammography units where the MGD for unit 1 was 2.0 ± 1.0 mGy for CC projection and 2.6 ± 1.8 mGy for MLO, and for unit 2, the MGD was 2.1 ± 1.0 mGy and 2.2 ± 1.0 mGy for CC and MLO projection views respectively.
The MGD for CC projection was found to be less than for MLO projection as in other studies done in Kenya and Bulgaria. The MGD for a 4.5 cm CBT for CC and MLO projections of 1.6 ± 0.1 mGy and 1.8 ± 0.01 mGy respectively were both less than 3.0 mGy recommended by the American college of radiology and the U.S Food and Drug Administration, 2005.
Conclusion
The MGD for a 4.5 cm CBT of 1.6 ± 0.1 mGy and 1.8 ± 0.01 mGy for CC and MLO projections respectively were both less than 3.0 mGy recommended by the American college of radiology and the U.S Food and Drug Administration, 2005. Hence the doses obtained were acceptable. Further studies should consider carrying out the study for a longer period to have a bigger number of patients, and therefore a wider variation in parameters, and also consider mammography units of different technical characteristics from different mammography centers for the establishment of national diagnostic reference levels.
References
- Wheeler Celeste. (2003, April). The Mammography Quality Standards Act: Misread Mammograms, Malpractice, and the Politics of Regulation.
- Uganda Breast Cancer Working Group (2003) Breast cancer guidelines for Uganda. Afr Health Sci 3: 47–50. [crossref]
- Rothenberg LN (1990) AAPM tutorial. Patient dose in mammography. Radiographics 10: 739–746. [crossref]
- American Cancer Society (ACS), 2014. Mammograms and Other Breast Imaging Tests.
- IAEA-TECDOC-1447 (2005) Optimization of Radiological Protection of the Patients: Image Quality and Dose in Mammography. ISBN: 92-0-102305-7
- American College of Radiology (ACR) (2014) Practice parameter for the performance of screening and diagnostic mammography
- IAEA-TECDOC-1067 (1999) Organization and Implementation of a National Regulatory Infrastructure Governing Protection against Ionizing Radiation and Safety of Radiation Sources. ISSN 1011-4289
- Dance DR, Skinner CL and Carlsson GA (1999) Breast dosimetry. Appl. Radiat. Isot. 50: 185–203.
- Elsie K, Gonzaga M, Francis B, Michael K, Rebecca N, Rosemary B, Zeridah M (2010). Current knowledge, attitudes and practices of women on breast cancer and mammography at Mulago hospital. Pan African Medical Journal. 5: 9
- IAEA Radiation Protection of Patients (RPOP).
- JS Wambani, GK Korir, MN Shiyanguya, & IK Korir (2011). Assessment of patient doses during mammography practice at Kenyatta National Hospital. East African Medical Journal.
- Simona Avramova-Cholakova and Jenia Vassileva.(2008). Pilot study of patient and phantom breast dose measurements in Bulgaria. Pol J Med Phys Eng 14: 21–32
- U.S Food and Drug Administration, (2005, September). Mammography Facility Surveys, Mammography Equipment Evaluations, and Medical Physicist Qualification Requirements under MQSA.